BACKGROUND AND AIMS
Pneumocystis jiroveci pneumonia (PJP) is an opportunistic infection affecting immunocompromised individuals. Its importance in patients without HIV has increased over the past decades due to the expanding armamentarium in immunosuppressive and chemotherapeutic therapies.1 Given its high mortality rate in non-HIV patients, PJP prophylaxis is commonly prescribed in many immunocompromising conditions and various guidelines have been established in oncology, bone marrow, and solid organ transplant.2-4 However, evidence regarding the burden of PJP and effectiveness of prophylaxis among patients with rheumatic symptoms remains limited. Epidemiological studies and guidelines for PJP prophylaxis in patients with rheumatic diseases are urgently needed. The objective of this study was to delineate the epidemiology, predictors of mortality, and efficacy of PJP prophylaxis among patients with rheumatic symptoms.
MATERIALS AND METHODS
The authors performed an observational, longitudinal cohort study based on data retrieved from the territory-wide electronic healthcare database (Clinical Data Analysis and Reporting System) of the Hospital Authority (HA).
HA is the sole public-funded healthcare provider in Hong Kong and covers over 90% of secondary and tertiary care of the 7 million population. All patients with a diagnosis of anti-neutrophil cytoplasmic antibody-associated vasculitis (AAV), immune-mediated myositis (IMM), rheumatoid arthritis (RA), systemic lupus erythematosus (SLE), systemic sclerosis (SSc), or spondyloarthritis (SpA) between 2015–2019 were included. Rheumatic diagnoses were defined based on diagnosis code using the International Classification of Diseases, Ninth Revision. Clinical information including patients’ demographics, medication prescriptions, blood tests, and mortality were recorded. Prevalence, prophylaxis, and mortality of PJP were calculated. Number needed to treat analysis was performed. Association analysis was performed to identify predictors of PJP-related mortality.
RESULTS
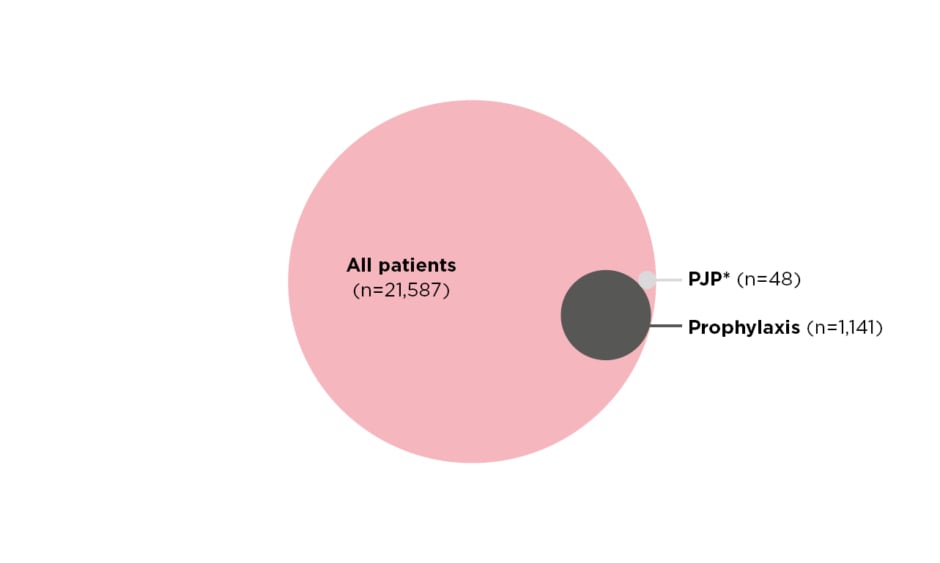
Over the period of 2015–2019, a total of 21,587 patients were included (54% RA, 25% SLE, 13% SpA, 5% IMM, 2% AAV, and 1% SSc). The majority of the patients were female (73.0%), and the mean age was 58±17.4 years. PJP prophylaxis was prescribed in 1,141 (5.3%) patients. PJP occurred in 48 (0.2%) patients. No patients who developed PJP received prophylaxis prior to infection (Figure 1).
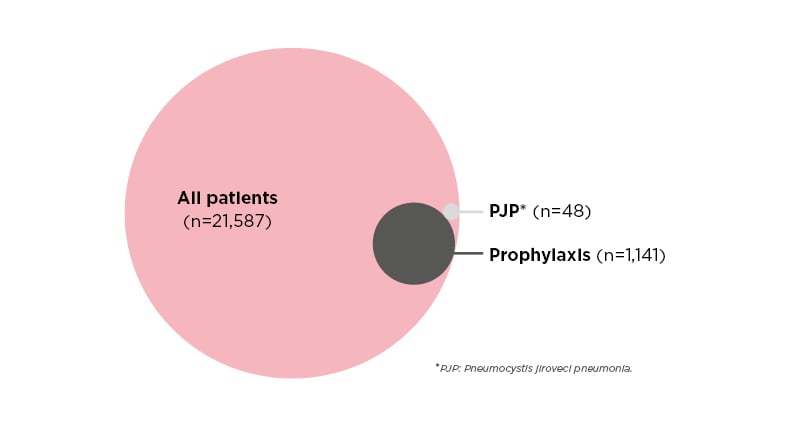
Figure 1: Proportional Venn diagram showing prevalence of pneumocystis jiroveci pneumonia and prophylaxis among patients with rheumatic disease.
The incidence of PJP was highest among patients with SSc, AAV, and IMM. The frequency of PJP prophylaxis prescribed based on physician’s discretion was also highest among patients with SSc, AAV, and IMM. Within these diseases, the majority of PJP occurred while patients were on glucocorticoids at daily prednisolone-equivalent doses of 15 mg/day or above. Using the number needed to harm of 135 for every severe adverse reaction as reference,5 PJP prophylaxis was effective in SSc, AAV, and IIM with number needed to treat analysis being 36, 48, and 114, respectively.
Overall, PJP has a mortality rate of 39.6%. In univariate analysis, lymphopenia and glucocorticoid dose at time of PJP diagnosis were associated with PJP-related mortality. In multivariate analysis, glucocorticoid dose at time of PJP alone was independently associated with PJP-related mortality (odds ratio: 1.09; 95% confidence interval: 1.02–1.64, p=0.02).
CONCLUSION
PJP is an uncommon but important infection among patients with rheumatic symptoms. PJP is associated with high mortality. Prophylaxis against PJP is effective and should be considered in patients with SSc, AAV, and IMM, especially those receiving glucocorticoid doses above P15. Glucocorticoid dose is independently associated with PJP-related mortality.