Abstract
Interventions such as exercise training and breathing strategies are components of pulmonary rehabilitation for people with chronic obstructive pulmonary disease (COPD); however, the conventional mode of gym-based exercise training may not be optimal for all individuals with COPD, and adaptive breathing strategies may be beneficial in reducing dyspnoea, but the current evidence is limited. Uptake and completion rates of pulmonary rehabilitation are suboptimal, so alternative interventions need to be considered. This review examines the current scientific evidence on alternative exercise and breathing interventions from systematic reviews, experimental and observational studies, clinical trial registries, and grey literature. Alternative interventions are assessed for the effect on exercise capacity and quality of life with the aim of guiding the development of strategies to increase training uptake and completion. Systematic reviews of tai chi, yoga, minimal or no equipment exercise, water-based exercise, inspiratory muscle training, and singing demonstrated positive effects on exercise capacity and/or quality of life compared to no training, with some interventions demonstrating comparable outcomes to conventional training. Some positive outcomes have been demonstrated for whole-body vibration, single-limb partitioning, and Nordic and downhill walking; however, further research is required to compare these interventions to conventional training. The most recent interventions examined include exer-gaming, virtual reality, dancing, and laughing; controlled studies are still required to determine the effect on patient outcomes. Although further research is needed to compare alternative exercise and breathing interventions with conventional exercise training, results to date are promising, suggesting that people with COPD will have more options that may help to improve training uptake and adherence.
INTRODUCTION
Chronic obstructive pulmonary disease (COPD) is recognised as a complex condition with effects extending beyond the respiratory system, including systemic manifestations1 and other comorbidities.2 This increased recognition and understanding of the multifactorial consequences of COPD and coexisting symptoms has led to a greater awareness of the importance of exercise training to reverse, manage, and/or improve physical function and health-related quality of life (HRQoL).3 Exercise training traditionally consists of a variety of land-based (most typically gym-based) lower and upper limb endurance and strength exercises to improve muscle function, reduce dyspnoea, increase exercise capacity, and improve HRQoL;3 however, the definition of exercise as an “activity requiring physical effort, carried out to sustain or improve health and fitness”4 lends itself to more than just the conventional modes of exercise training characteristic of pulmonary rehabilitation (PR) programmes worldwide, such as cycling and treadmill walking.5 Alternative exercise training modes, such as water-based exercise (WBE) training and tai chi, have now also been used to improve exercise capacity and HRQoL in people with COPD.6,7
Breathing strategies are another component of PR for people with COPD. Breathing strategies focus on retraining to slow the respiratory rate through prolonged expiration3 and, traditionally in PR, using breathing retraining strategies to reduce dyspnoea, such as yoga breathing or pursed-lips breathing.3 Breathing retraining extends to more than just these breathing strategies and could be achieved through singing or laughing.
Uptake and completion rates of PR are suboptimal,8 and the presence of comorbidities has been attributed to the non-completion of PR.9 Incorporating the values and preferences of people with COPD is essential in evidence-based decision making and delivering patient-centred care.10,11 Therefore, there is now growing interest in investigating alternative exercise and breathing interventions in people with COPD, which may address these issues.12-14
The purpose of this study was to identify, highlight, and critically review current and new literature investigating alternative exercise and breathing interventions in people with COPD that aimed to improve exercise capacity and/or HRQoL. The results will help guide the development of strategies to increase the uptake and completion of exercise training.
METHODS
An alternative exercise intervention was defined as an activity that required physical effort other than conventional cycling and walking exercises recommended for people with COPD.3 An alternative breathing intervention was defined as an activity that required physical effort other than the conventional yoga breathing or pursed-lips breathing typically included in PR programmes.3 These interventions were identified by a number of sources, including expert consensus, review of published narratives, expert reviews of PR and exercise training, and texts of PR. The primary inclusion criteria for this review was that, in people with COPD, the alternative exercise and breathing interventions needed to be supervised and be an activity that required physical effort.4 The secondary inclusion criteria were studies that included an outcome measure of exercise capacity (peak, endurance, or functional exercise capacity) and/or HRQoL, with a study duration of at least 4 weeks.15 Studies were excluded if the mode of training was provided as an adjunct to conventional PR (not in isolation) or were not available in English.
The literature search process is detailed in Table 1.16 Multiple types of literature were considered (in a hierarchical nature) to ensure all identified alternative interventions were highlighted to provide information on the current state of evidence (planned, in progress, or currently available). Literature searches were undertaken by one review author for each alternative intervention. A second author reviewed the results of each search and consensus was reached by discussion to ensure no pertinent studies were overlooked.
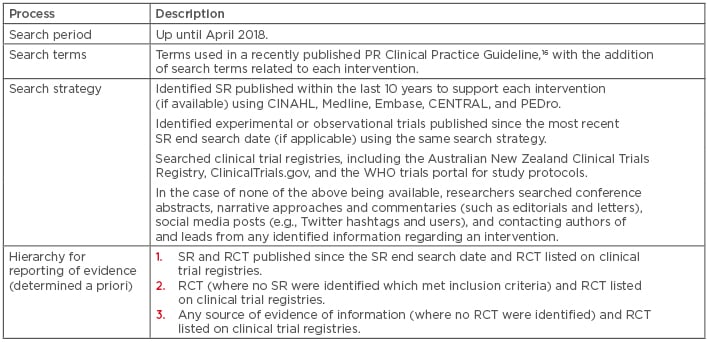
Table 1: Literature search process.
PR: pulmonary rehabilitation; RCT: randomised controlled trial; SR: systematic review; WHO: World Health Organization.
RESULTS
Fourteen interventions that met the primary inclusion criteria were identified, including tai chi, yoga, minimal or no equipment exercise, WBE, whole-body vibration (WBV), single-limb partitioning, Nordic walking (NW), downhill walking (DW), exer-gaming, virtual reality, dancing, inspiratory muscle training (IMT), singing, and laughing. The description and rationale underpinning each alternative exercise intervention is presented in Table 2,6,7,17-29 with breathing interventions presented in Table 3.30-33
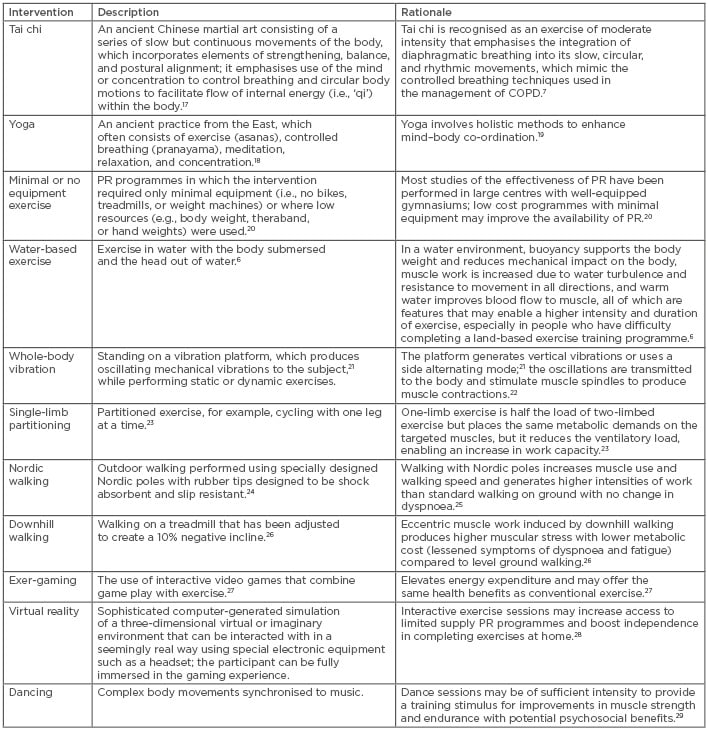
Table 2: Description and rationale for alternative exercise interventions.
COPD: chronic obstructive pulmonary disease; PR: pulmonary rehabilitation.
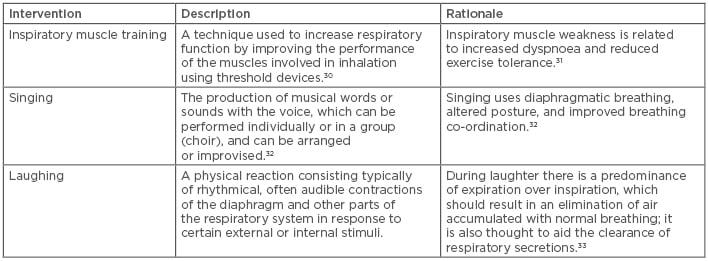
Table 3: Description and rationale for alternative breathing interventions.
Alternative Exercise Interventions
Tai Chi
A Cochrane review published in 2016 included 12 randomised controlled trials (RCT) (N=811) investigating tai chi training of 6–52 weeks duration.7 Assessing 6 studies (n=318), compared to no exercise training, tai chi demonstrated a larger improvement in 6-minute walk distance (6MWD) (mean difference [MD]: 27 m; 95% confidence interval [CI]: 11–49 m).7 In one study (n=60), a comparison of tai chi and breathing exercises versus breathing exercises alone found no superiority for functional exercise capacity or HRQoL.7 No adverse events were reported.7 An additional 12-week RCT comparing tai chi to PR was published in 2018, with comparable improvements in exercise capacity and HRQoL immediately following a 12-week intervention.34 At 3 months post intervention, there was a significant difference in HRQoL favouring tai chi.34
Clinical trial registry searches found four RCT with a tai chi programme duration ranging from 12–24 weeks: tai chi versus conventional exercise versus usual care; tai chi versus group walking versus usual care; tai chi versus conventional exercise; and tai chi versus breathing exercise versus education. The study protocols of two of the four trials have been published.35,36
Tai chi training is safe and feasible in people with COPD. Tai chi has different styles, each with its own characteristics and forms. Exercise intensity, duration of practice, and length of programme often varies between styles. New trials will provide more insight into the effect of tai chi compared to active training interventions, and future trials are required to determine the long-term benefits.
Yoga
A systematic review (SR), including studies published up to June 2017, included a total of 10 trials (8 RCT and 2 non-RCT) (N=312) investigating yoga training of 12–36 weeks duration.19 Yoga with or without education was compared to controls, including usual medical care, PR, or education.19 In six studies of 312 participants, yoga demonstrated a larger improvement in 6MWD compared to controls (MD: 22 m; 95% CI 10–34 m). Improvement was also found regarding the St George’s Respiratory Questionnaire (SGRQ) total score in three studies of 105 participants compared to controls (MD: -3.81 points; 95% CI: -6.65 to -0.97 points).19 No adverse events were reported.19 An additional RCT of 12 weeks of yoga training compared to PR was published in 2017, with comparable improvements in exercise capacity and HRQoL after intervention.37 Clinical trial registry searches did not find any further trials meeting the inclusion criteria.
Evidence to date indicates that yoga is safe and feasible in people with COPD. Despite evidence of improvements in exercise capacity and HRQoL, these did not reach the minimal important difference (MID) for 6MWD38 or SGRQ total score.39 In addition, non-RCT were included in the SR,19 and some studies investigating yoga training included controlled breathing (pranayama) only, while some studies included exercise, meditation, and relaxation in addition to controlled breathing.19 Similarly to tai chi, yoga has many different forms and styles, which can easily be modified to suit individual needs; however, the exercise intensity may vary between styles. These variations limit the ability to draw a clear conclusion on the effect of yoga training in people with COPD.
Minimal or No Equipment Exercise
A SR has shown that PR with little or no equipment improved exercise capacity and HRQoL when compared to no training in people with COPD.20 In the eight studies reviewed (N=285), there were significant improvements reported in HRQoL and both 6MWD and incremental shuttle walk distance,20 with only the 6MWD reaching the MID.38 The training provided included ground-based walking, NW, and different modes of strength training, including free weights, therabands, sit-to-stand exercises, and stepping,20 rather than the conventional exercise training that uses bikes, treadmills, and weight machines.3,5 The frequency of supervision provided ranged from three times per week to once per month, and the programmes were home-based, varying in length between 4–12 weeks.20 A Cochrane review protocol was published in 201740 and clinical trial registry searches revealed one RCT from Switzerland examining the effects of a long- term home-based exercise training programme using minimal equipment versus usual care.41
These results provide support for supervised exercise training using minimal or no exercise equipment when compared to no exercise training in people with COPD. Further research with larger cohorts and comparison of supervised training with no equipment to conventional exercise training will strengthen the evidence.
Water-Based Exercise
A Cochrane review published in 2013 included five RCT (N=176) investigating WBE training of 4–12 weeks duration compared with no exercise training and/or land-based exercise (LBE) training.6 Compared to LBE training, WBE improved the endurance shuttle walk distance (MD: 313 m; 95% CI: 232–394 m) and the fatigue domain of HRQoL.6 Other aspects of HRQoL were not significantly different between WBE and LBE.6 One minor adverse event was reported.6 An additional RCT of 6 months that compared WBE and LBE training was published in 2018, with comparable improvements in exercise capacity and HRQoL between the two training groups.42 Clinical trial registry searches did not locate any further studies.
One trial in the aforementioned Cochrane review specifically included people with COPD with physical comorbidities, such as musculoskeletal conditions, joint replacements, neurological conditions, and obesity,43 indicating WBE may be particularly suitable for people with physical limitations to exercise on land. WBE may not be acceptable to all people with COPD, with two studies reporting that three participants refused to consider WBE.6 Conversely, two studies reported participant subjective preference for an exercise training environment, with WBE preferred by the majority over LBE (49% versus 37%, respectively).6
WBE is safe and improves exercise capacity and HRQoL, with a greater effect on improving endurance exercise capacity over LBE training. Long-term effects of WBE have not yet been investigated.
Whole-Body Vibration
Three SR,21,22,44 with a combined total of six studies, have been published on WBV for people with COPD; however, all reviews included studies of <4-weeks duration and thus did not meet the criteria for inclusion in this review. Despite this, the three reviews reported no serious adverse events from WBV.21,22,44
Four RCT of at least 4-weeks duration of WBV have been published. Significant improvements in 6MWD of 80 m (95% CI: 68–92) following a 6-week WBV training programme involving static work of the lower limbs on a vibration platform were found when compared to lifestyle and physical activity advice alone.45 Smaller improvements in 6MWD were also shown in a small (N=11) 12-week cross-over pilot study with a comparison group of no intervention,46 and in a 3-month WBV programme compared to breathing retraining and calisthenics.47 However, following a 3-month training period comparing WBV to resistance training, there were no differences between groups for 6MWD.48 Improvements in HRQoL also did not reach significance between WBV and comparison groups.46-48 A review of the clinical trial registries identified four studies currently recruiting participants with COPD for WBV, with a further eight studies listed as having completed recruitment.
The role and benefit of WBV in COPD appears promising for improving functional exercise capacity, with further research occurring. This may assist in determining the optimal mode, frequency, and duration of WBV delivery.
Single-Limb Partitioning
One RCT34 and one small non-controlled study49 investigated one-legged cycling for people with COPD. Both studies demonstrated that a 7-week or 8-week one-legged cycling programme improved peak oxygen uptake.23,49 In a pragmatic feasibility trial of implementing one-legged cycling training as the principal aerobic exercise activity in PR, the 6MWD improved by a mean of 72 m (95% CI: 45–98), and a change in HRQoL above the MID was found.50
Clinical trial registry searches identified one RCT of single-limb resistance training compared to two-limb resistance training. Given the two previous studies in the area were published nearly a decade ago, the results of this study will add new knowledge to this area.
Nordic Walking
One RCT was identified investigating NW in people with COPD. A 12-week training programme of NW compared to no training in people with COPD (n=60) showed an increase in 6MWD24 with the results maintained at 9 months follow-up and with a 92% completion rate.24 A search of the clinical trial registries did not find any further studies.
Although the evidence is limited, the available study reported that supervised NW was safe, suggesting it may be an accessible and low-cost mode of training that may enhance long-term adherence to exercise and could be ideal for people with COPD who prefer to exercise outdoors. Further studies are required to confirm or refute this hypothesis.
Downhill walking
One RCT investigated DW in people with COPD.51 Thirty-four people were randomised to 12-weeks of DW or conventional level walking.51 Similar improvements were observed between the two groups for change in 6MWD and cycle endurance.51 More participants in DW (94%) exceeded the 6MWD MID38 compared to level walking (65%).51 Importantly, fewer symptoms were reported during DW training.51 No further trials were found on the clinical trial registries. This one study provides evidence of an effect of DW on exercise capacity. Further studies are warranted to confirm and further examine the effect of DW.
Exer-Gaming
One uncontrolled study using gaming technology has been reported in people with COPD using the Nintendo Wii Fit programme, which allows participants to complete endurance training of the upper and lower limbs (e.g., jogging-based movements) as well as functional upper and lower-limb exercises (e.g., squat, stepping activities, and boxing).27 Eighteen participants with moderate-to-severe COPD completed training in the home environment with exercise on most days per week over a 12-week period.27 A significant increase in endurance shuttle walk test time of 131±183 seconds, a significant increase in the total score of the Chronic Respiratory Disease questionnaire, and no adverse events were reported.27 Searches of clinical trial registries yielded no further studies. This preliminary evidence suggests that exer-gaming as a form of exercise training is feasible and may be effective in this population.
Virtual Reality
Given that virtual reality technology is relatively new to the gaming world, no peer-reviewed publications or clinical trial registry listings examining the feasibility or effectiveness in people with COPD were identified. However, a virtual reality application has been developed by researchers at Manchester Metropolitan University, Manchester, UK for people with COPD.28 The app contains a virtual beachside training environment where participants can interact in an exercise class, performing exercises from the comfort of their own homes. This application is currently being evaluated for ease of use and acceptability by people with COPD.
Dancing
There is currently no evidence on the effect of dancing in people with COPD. However, a recent pilot study (N=5) indicated three expert-led dance sessions may provide a suitable training intensity for people with COPD.29 People with chronic lung diseases, including COPD, have also expressed interest in participating in dance-based PR.52 Dance in COPD will be an emerging field of research, with investigators in Canada currently examining the feasibility of dance as an intervention.53 It is anticipated that findings from this study will inform design for a future RCT.
Alternative Breathing Interventions
Inspiratory Muscle Training
In a recently published SR of IMT, 29 RCT, non-RCT, and cohort studies investigated constant-load threshold IMT with a duration range of 4 weeks–12 months compared with sham IMT, general exercise training, incentive spirometry, education, respiratory muscle stretch gymnastics, expiratory muscle training, and usual care.45 IMT significantly improved 6MWD which surpassed the MID.30 The meta-analysis result from nine studies for HRQoL failed to reach a statistically significant improvement.30 One further RCT has been published since the end search date for the SR. Eight-weeks of IMT compared to sham training control significantly increased endurance exercise time.54
Clinical trial registry searches found numerous research activity in this area with 11 studies currently recruiting participants, and an additional two studies not yet recruiting. Effects of IMT in HRQoL need to be examined further, as well as determining the optimal prescription for IMT training.
Singing
A Cochrane review published in 2017 included three RCT (N=112) investigating singing for 6–24 weeks duration compared with control (film workshop, handcraft work, or no intervention).32 In two studies (N=52), compared to the control group, singing improved HRQoL (SF-36 Physical Component Summary score MD: 12.64; 95% CI: 5.50–19.77), but not SGRQ total score.32 Singing had no impact on exercise capacity.32 No adverse events or side effects were reported, and no studies examined long-term outcomes.32 Clinical trial registry searches located one study currently recruiting participants to 10-weeks of singing training compared to PR.
Qualitative research studies have reported high satisfaction with singing by people with COPD;55 however, the optimal dosage to achieve positive outcomes is yet to be determined.32
Laughing
There is currently no evidence on the effect of laughing in people with COPD. However, a single laughter intervention improved cheerfulness,56 and a sense of humour has been associated with an enhanced HRQoL in people with COPD.33 Clinical trial registry searches revealed no studies on this intervention.
DISCUSSION
This review investigated the research around novel interventions of exercise and breathing to improve exercise capacity and/or HRQoL in people with COPD. SR of tai chi, yoga, minimal or no equipment exercise, WBE, IMT, and singing have demonstrated positive effects on exercise capacity and/or HRQoL compared to no training, with some interventions demonstrating comparable outcomes to conventional exercise training. Some positive outcomes have been demonstrated for WBV, single-limb partitioning, NW and DW; however, further research is required to compare these interventions to conventional exercise training. The newest exercise and breathing interventions to be examined include exer-gaming, virtual reality, dancing, and laughing, and controlled studies are required to determine their effect on patient outcomes.
The purpose of identifying alternative exercise and breathing interventions is to widen the options available to people with COPD to improve their exercise capacity and HRQoL. In rural and remote locations, and in centres with limited funding and facilities, lack of conventional exercise equipment may be a barrier to setting up conventional PR programmes, as well as a barrier for patients when asked to perform home exercise. Minimal or no equipment training could address these problems. People with physical comorbidities, such as musculoskeletal conditions, often find conventional gym-based exercise difficult or aggravating to their condition, so the appeal of reduced weight-bearing training, such as WBE,43 or breathing interventions, such as singing, may be appealing. Preliminary evidence on sophisticated gaming technology suggests that it can be effective for people with COPD27 and may help to engage people in exercise training, but more studies are required to verify these results.
Limiting factors to implementing some alternative interventions are the need for specialised equipment and skilled personnel. For example, a limitation to the use of DW as part of an exercise programme is the need to have a specialised treadmill. More research is needed in this area to determine if DW using ramps and hills would provide the same training effect as conventional treadmill training. Specialised equipment is also required for NW and WBV, access to technology is required for exer-gaming and virtual reality, and WBE requires access to a pool. Specialised personnel or training of existing PR staff in new skills is required to deliver tai chi, yoga, NW, singing, and dancing.
There are some limitations to the evidence reviewed in this paper for the different interventions. It is unclear whether this evidence can be applied to people with different severities of COPD or those on long-term oxygen, or use these interventions for maintenance of health outcomes after completion of conventional training. Some of the evidence is from non-controlled studies, and not all studies compared the alternative intervention to conventional training; therefore, it cannot be concluded that these alternative interventions can replace conventional training. Rather, the evidence presented here supports new interventions that could be offered to improve exercise capacity and HRQoL in people with COPD. Furthermore, this review did not examine the issue of delivery of the interventions in different environments, such as hospital centres, community centres, and the home environment. Future steps would be needed to investigate the feasibility of offering and implementing these alternative interventions in different settings and to determine the acceptability of these interventions in routine clinical PR practice. Certainly, this issue has been established for some alternative interventions such as no equipment exercise,57 single-limb partitioning,50 and WBE.58
It is well established that PR should encompass patient-tailored therapies that are individually designed to improve the physical condition of people with COPD, and meet the unique needs of the patient, including disease severity, complexity, and comorbidities.3 With emerging evidence on alternative interventions, clinical practice needs to move beyond offering only conventional exercise training options. The provision of a menu of interventions to improve exercise capacity and HRQoL for people with COPD gives patients options that may be better suited to their physical capacity and preference. It is well established that, in certain global areas, the access to conventional exercise training is suboptimal.8 Offering options and a choice of interventions may increase the appeal of exercise training and improve the rates of referral, uptake, and retention. Additionally, more options and a flexible model would allow patients to select their preferred intervention and to transfer between different interventions to improve their physical condition whilst maintaining their level of interest in exercise training.
CONCLUSION
The results of the studies reviewed have shown that different exercise and breathing interventions are safe and effective in improving exercise capacity and/or quality of life in people with COPD. In many cases further research is needed to compare the interventions to conventional exercise training, but the results to date are promising, suggesting that in the future people with COPD will have greater options available for exercise training and breathing interventions, and may be offered a choice of ways to manage their condition, which may lead to increased uptake and completion of training.








