BACKGROUND
Latest guidelines in pulmonary arterial hypertension (PAH) recommend the use of multi-parameter risk assessment at both diagnosis and follow-up to guide treatment.1 A new model, REVEAL 2.0, has recently been developed by the US Registry to Evaluate Early and Long-Term PAH Disease Management (REVEAL) investigators.2 Their original model, derived from a large multicentre cohort in the USA3 and based on 12 variables (demographic, disease subtype, comorbidities, vital signs, biochemical, functional, echocardiographic, haemodynamic, and pulmonary function assessments), has been updated to include hospitalisations, and is designed for use during patient follow up.2,4 REVEAL 2.0 divides patients into eight separate risk strata, or three simplified strata (low, intermediate, and high risk). The aim of this analysis was to assess the prognostic performance of the REVEAL 2.0 risk score applied to a large external cohort of patients with PAH from the Pulmonary Hypertension Society of Australia and New Zealand (PHSANZ) Registry.
METHODS
The PHSANZ registry includes 2,736 patients with clinician-diagnosed Group 1 PAH enrolled from 21 specialist centres from Australia and New Zealand.5 Prospective data collection began in December 2011, and like the REVEAL registry,3 includes all Group 1 PAH subtypes and both prevalent and incident cases. REVEAL 2.0 risk scores were calculated for individual patients from the PHSANZ registry at 12 months post-enrolment. Scores were determined based on most recent investigation results, using an identical process to the REVEAL 2.0 analysis.2 Kaplan–Meier survival estimates were calculated up to 60 months for each REVEAL 2.0 risk group for both eight strata and three strata models. A sensitivity analysis was performed using an incident-only cohort. The model’s ability to discriminate likelihood of survival was determined using Harell’s c-statistic.6
RESULTS
In total, 1,011 PAH patients in the PHSANZ registry had sufficient data to permit application of the REVEAL 2.0 model.4 Most (75.0%) were previously diagnosed cases. Using 1-year post enrolment as the baseline, overall 12 and 60-month survival for the PHSANZ cohort was 91.3% (95% confidence interval [CI]: 89.4–93.0) and 65.3% (95% CI: 61.6–68.8), respectively. The REVEAL 2.0 model effectively discriminated risk in the large external PHSANZ registry cohort, with c-statistic 0.74 (both for full eight-strata and three-strata models). When applied to incident cases only, c-statistic was 0.73. The three-category REVEAL 2.0 model demonstrated robust separation of 12 and 60-month survival estimates (all risk categories comparisons p<0.001) (Figure 1). Although the full eight-tier REVEAL 2.0 model separated low, intermediate, and high-risk patients, survival estimates overlapped within the intermediate and high-risk strata.
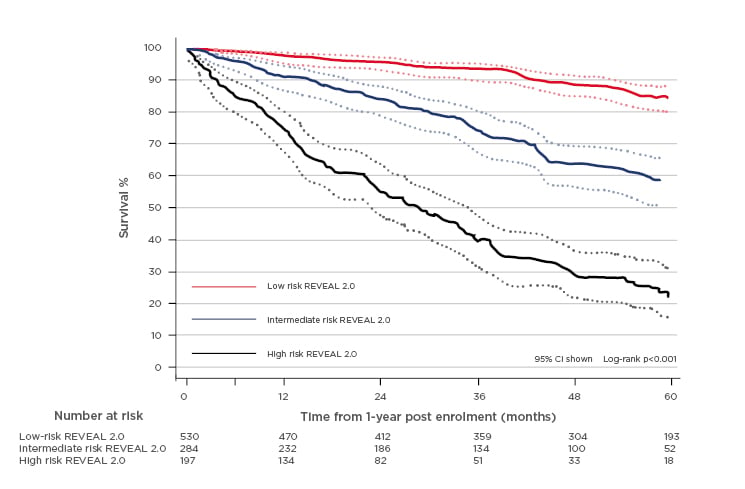
Figure 1: PHSANZ survival by REVEAL 2.0 risk category.
CONCLUSION
This study represents the first external validation of the REVEAL 2.0 model supporting its clinical use in risk assessment of PAH patients at follow-up. The model achieved clear separation of survival estimates by 12 months in a mixed prevalent and incident cohort. As discussed at the recent European Respiratory Society Congress in Madrid, prospective validation and comparisons with other prognostic models, such as those based on the 2015 European Society of Cardiology/European Respiratory Society (ESC/ERS) guidelines, is now needed.








