BACKGROUND
Bronchiectasis is a chronic respiratory condition that has a significant impact on morbidity, quality of life, mortality, and healthcare services.1 The current aims of therapeutic management are preservation of lung function, reduction of exacerbations, minimising complications, and improving quality of life.2,3 The British Thoracic Society (BTS) guidelines suggest a five-step plan to treat patients with bronchiectasis, ranging from Step 1, which includes all patients, to Step 5, which is specific to those with worse symptoms.3 Therapeutic strategies and interventions common to most international guidelines include antibiotics, airway clearance techniques, and pulmonary rehabilitation.2,3 The aim is to break the vicious recurrent cycle of infection, inflammation, impaired mucociliary clearance, and structural lung damage. Self-management (SM) has been recommended in clinical guidelines as an important intervention that could potentially empower patients to manage their condition, reduce exacerbations and therefore disease burden, and improve quality of life.3 Yet, to date, there is very little evidence to support SM programmes for patients with bronchiectasis, despite being a recommendation in Step 1 of the BTS guidelines. A previous Cochrane systematic review found insufficient evidence to determine whether SM interventions benefit patients with bronchiectasis,4 which has since been confirmed by a broader review.5
METHODS
Three focus groups of 17 adults with bronchiectasis were conducted at three National Health Service (NHS) sites in North West England, UK. Additionally, semi-structured interviews were undertaken with 11 healthcare professionals (HCP), including doctors, nurses, and physiotherapists. Thematic analysis identified key findings which were verified by independent audit. This study was approved by NHS London Harrow Research Ethics committee (ref 18/LO/1671).
RESULTS
Four key and common themes were identified from both HCP and patients: what is SM?; influencers of SM; benefits of SM; and barriers to SM (Table 1). When considering what SM is, both groups recognised similar components of SM. Sub-themes varied among the groups, with patients highlighting that SM was about learning what works for you, and how it can be used to moderate behaviour. HCP focussed on delivery and structure of SM and resources. Influencers for engaging in SM were recognised by HCP as individual patient attributes in addition to the knowledge and skills of HCP. Both groups saw distinct benefits to SM, namely treating and preventing exacerbations and controlling anxiety, and, from the patients’ perspective, as a proxy for HCP; HCP focussed on clinical outcomes, empowering patients and improving economic benefits to healthcare delivery. Patients and HCP recognised common barriers, but only patients referred to SM as time-consuming. Both groups recognised the importance of access (or lack of) to resources including HCP’s knowledge of the condition.
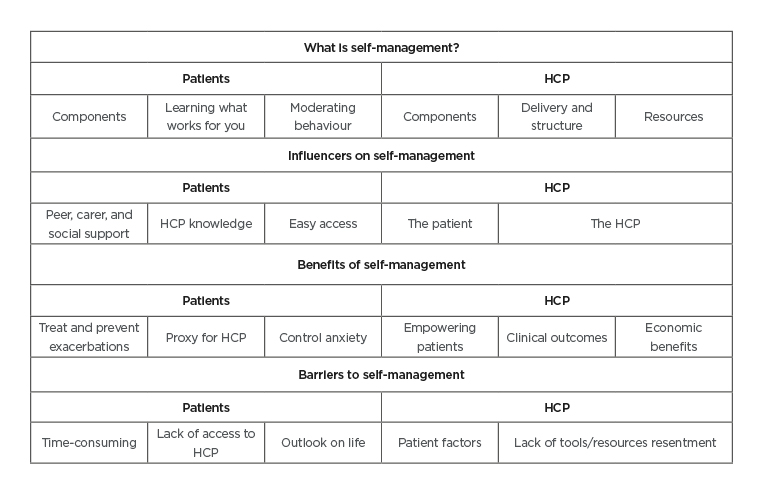
Table 1: Key themes and subthemes for patients and healthcare professionals.
HCP: healthcare professionals.
Patients did not refer to distinct traits in themselves that may influence engagement in SM, but demographics gave insight into activity levels relating to SM.Patients valued peer learning whilst HCP acknowledged individuals’ need for different approaches and it’s not one size fits all.
SUMMARY
Both patients and HCP had common insights about SM for patients with bronchiectasis. All participants were positive about SM, but barriers were identified that provided a vital insight necessary to the design of future programmes. Findings from this study suggest that patients’ psychosocial and socioeconomic circumstances may affect adoption and activation of SM behaviours.








