BACKGROUND AND AIMS
The role of barium swallow in the diagnosis of upper gastrointestinal tract diseases has been overshadowed in the last few years, and for many reasons. Important improvements in diagnostic technologyhave gradually led classic barium radiography to hold a lesser role.1 In fact, the internationally recognised diagnostic gold standard for achalasia,2,3 the topic of this study, is the high-resolution manometry evaluation, which allows the diagnosis and staging of achalasia according to the Chicago classification. Considering the aim of radiologists, which should be to innovate on a daily basis without forgetting about techniques that are effective, available, and easy to perform, such as barium swallow,4 the authors designed a study to establish a new radiographic grading system for achalasia; this was named the FBF score (from the name of the corresponding institution: FateBeneFratelli, Benevento, Italy). The score is totally congruent with the Chicago classification assumptions and allows for more accurate and clinically oriented prognostic grading, especially precise subtype diagnoses, completely comparable to manometric ones, using the authors’ in-house barium swallow protocol.5,6
MATERIALS AND METHODS
The authors started to develop their FBF scoring system by profiling the three achalasia subtypes described in the clinical/manometric Chicago classification (I: hypotonic; II: panpressurising; and III: spastic) into three equivalent radiographic grades; this was done using five morphodynamical findings as scoring criteria: bird-beak sign (2 points), lumen dilation (2, 4, or 6 points, respectively, for a lumen calibre of <4 cm, 4–6 cm, >6 cm), hypotonia (2 points), stasis (2 points), and spasm (-2 points). The score, ranging 0–12, is calculated by adding up the points from each finding (if found). Scores 0–6 are considered FBF/Chicago Subtype III, while scores 6–8 are considered Subtype II (except score 6, with spasm, which is considered Subtype I) and scores of >8 are consistent with Subtype I.
Between June 2017 and June 2020, 141 patients (mean age: 59.2 years; male: 60.2%; female: 38.8%), already diagnosed with achalasia using high-resolution manometry, were evaluated with dynamic barium swallow. They then received blinded review by two radiologists who had gastrointestinal experience, and were subsequently graded using the FBF score. Radiographic grading accuracy and sensitivity were evaluated using manometry data as gold standard. The five scoring criteria were each evaluated for sensitivity and specificity with regard to each radiological grade.
RESULTS
The FBF score allowed the authors to predict the clinical/manometric subtype with high accuracy, with sensitivity values reaching 91.30% for Subtype III, 95.40% for Subtype II, and 98.03% for Subtype I, the latter being correctly diagnosed in 50/51 patients with FBF ≥8 (presence of ≥4 combined radiographic findings). Spasm showed high specificity in Subtype III (95.65%), while stasis resulted in high sensitivity for Subtype II (93.18%).
CONCLUSION
Radiographic grading of achalasia using the FBF score was shown to be highly sensible and accurate when compared to the manometry results, especially in Subtypes II and III. FBF score implementation might allow more precise morphodynamical analysis, structured reporting, and better overall diagnostic support for manometry, patient stratification, and therapeutic choices. It should be noted, however, that this study is monocentric and the patient number is limited (141); even though preliminary data suggest a substantial comparability between barium swallow plus FBF score and high-resolution manometry, further studies are needed for a complete validation. ■
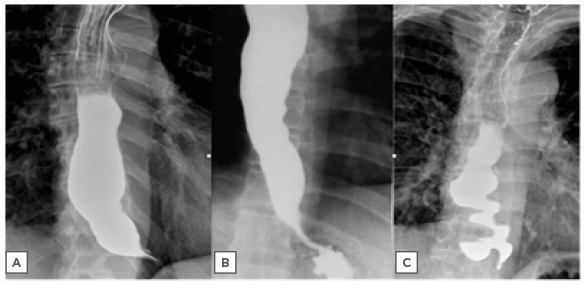
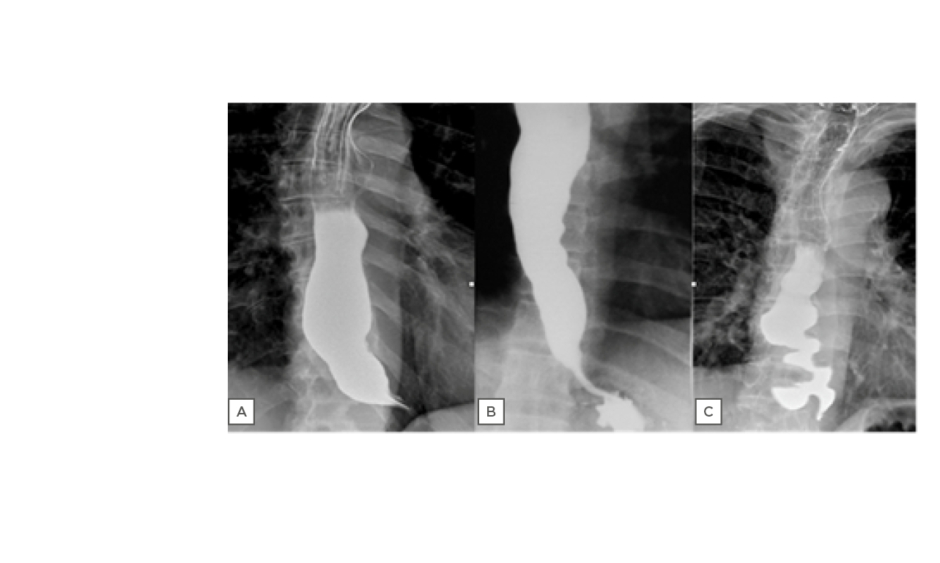
Figure 1: Radiologic profiles of achalasia subtypes: A) hypotonic, Subtype I; B) panpressurising, Subtype II; and C) spastic, Subtype III.