Abstract
Neurological symptoms such as headache and blurring of vision could be a manifestation of an underlying lung adenocarcinoma. The objective of this case report is to unveil the possible differentials and processes involved in the diagnosis of marantic endocarditis. A 57-year old male with blurring of vision and brain CT revealing multiple abscesses, sterile on culture, was treated as per guidelines. However, the patient had recurrent complaints that reinforced recurrent admissions and the patient was found to be COVID-19 positive during the pandemic when a routine test was performed in the emergency department. Suspicious lesions on the chest X-ray were further scrutinised and the patient was diagnosed with lung adenocarcinoma. To further investigate the sterile cultures in the brain, a cardiologist’s opinion was taken and a transthoracic echocardiogram was done, which was unremarkable. The increased suspicion for non-infective endocarditis necessitated a transoesophageal echocardiogram, which was positive for vegetations on the aortic valve. The patient was treated with anticoagulants and chemotherapy. In conclusion, in patients with CT findings of abscesses and sterile cultures, it is crucial to investigate the possible differentials in a meticulous fashion, as there could be an undiagnosed lung cancer in a non-smoker and there is a rare possibility of a sterile vegetation on the aortic valve, as was seen in the authors’ case.
Key Points
1. The case highlights the importance of a comprehensive evaluation and a high degree of suspicion in the evaluation of patients with some peculiar features for non-bacterial thrombotic endocarditis such as lung adenocarcinoma, sterile cultures, and a positive transoesophageal echocardiogram.
2. The case also demonstrates the conundrums that arose while evaluating a patient for a headache and blurring of vision. Thus, one of the differentials for headache with a CT scan demonstrating ‘abscesses’ that should be considered, if sterile, is the possibility of non-bacterial endocarditis.
3. Transoesophageal echocardiogram shows higher accuracy in detecting non-bacterial thrombotic endocarditis compared to transthoracic echocardiogram.
INTRODUCTION
Non-bacterial endocarditis (also known as marantic endocarditis), a term coined by Gross and Fiedberg in 1936,1 encompasses the non-infectious (sterile) vegetations on structurally normal or superficially damaged cardiac valves in the absence of blood stream infection.2 Studies have postulated that local physical damage or cytokine mediated damage leads to platelet consumption, activation of clotting factors, and interlacing of fibrin strands that could be contributing to the vegetation formation.2,3
Embolic spread is seen in approximately 50% of patients with non-bacterial thrombotic endocarditis (NBTE), while 42% of NBTEs are associated with malignancies and 33% with neurological manifestations.4 Other commonly involved vessels include cerebral, coronary, mesenteric, and digital vessels.5,6 Being a non-inflammatory vegetation, the emboli are released with minimal changes in the valves, further making the diagnosis challenging.3
Lung adenocarcinoma, which is considered one of the potential causes of marantic endocarditis, has been explored in the case report. When diagnosed at advanced stages, the prognosis of patients with lung cancer is very poor, with a 5-year survival of 12%, while the more distant metastases lead to a survival rate of less than 5%.7
The presenting complaint of patients with marantic endocarditis could be a distant metastasis.8 Thus, the authors present complexities of a case of lung adenocarcinoma, which was incidentally suspected while screening for COVID-19. Marantic endocarditis increased suspicion and the foremost clue to the quandary, a simple headache proving to be a brain metastasis, instigated the whole investigative process.
CASE PRESENTATION
A 57-year-old male patient, known to have hypertension, presented with complaints of blurring of vision involving both eyes for 3 weeks. They also had an episode of loss of consciousness after a fall from a vehicle approximately 15 days previously. After the episode, they had a headache and an episode of vomiting. They were haemodynamically stable.
On ophthalmological examination, the uncorrected visual acuity of the right and left eye was 6/18 P (the smallest row of letters that a normal eye could discern at 18 m is what the tested eye can discern at 6 m) and 6/12 P (the smallest row of letters that a normal eye could discern at 12 m is what the tested eye can discern at 6 m), respectively. Non-contact tonometry revealed a pressure of 15/16 mmHg, pupils were round and reactive, and fundoscopic examination and extraocular movements were unremarkable. Neurological examination revealed no focal deficits.
CT of the brain reported two hypodense ring enhancing lesions with disproportionate oedema at the post-parietal region with mass effect. Differential diagnosis included abscesses or secondaries from a malignancy. Subsequently, a neurosurgical evaluation required a surgical approach by a burr hole bilaterally in the occipital region. With the patient in prone position, a bilateral linear incision was traced and a burr hole was marked. Under navigation guidance, the abscess was drained and sent for cultures. Wound closure was done in layers. The cultures, both in aerobic and anaerobic media, revealed no growth. On a follow-up visit after 1 week, complaints of headache and blurring of vision persisted.
A repeat brain CT at this time reported a persistent perifocal oedema along the bilateral parieto-occipital region with hypodensities (residual abscess). No interval change in the mass effect on the underlying brain parenchyma was seen, although a midline shift to the left by approximately 8 mm was reported. No other significant abnormalities were observed. The following day, bilateral exploration of the abscess was performed with the patient in prone position, with head placed on a horse shoe. Bilateral incision was deepened and under navigation guidance, the abscess was drained. A thorough vancomycin and gentamicin wash was given until fluid appeared unremarkable. Bilateral scalp wounds were sutured and dressed. Consequently, the patient reported a complete recovery of their initial symptoms. The cultures performed in both aerobic and anaerobic media revealed no growth. Gram stain and acid-fast bacilli were negative as well.
On their visit to the emergency department after approximately 1 month, the patient reported complaints of blurring of vision, headache, and a generalised weakness. In view of the ongoing pandemic of COVID-19, they were tested for the same, and turned out to be positive. They were then admitted to the COVID-19 ward. Chest X-ray revealed mediastinal lymphadenopathy (Figure 1), which necessitated a high resonance CT (HRCT) of the chest. This further revealed a neoplastic right hilar and right lower lobe soft tissue, enlarged mediastinal adenopathy, and multiple pulmonary metastases along with mild pericardial effusion (Figure 2).

Figure 1: Chest X-ray showing right sided hilar lymphadenopathy.
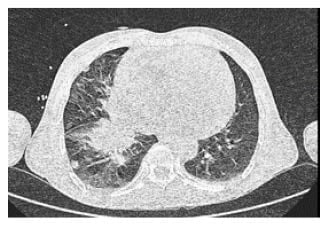
Figure 2: High resolution CT of the chest showing neoplastic right hilar lymphadenopathy and right lower lobe soft tissue and pericardial effusion.
A whole body CT scan with contrast revealed a neoplastic right hilar and right lower lobe soft tissue and mediastinal lymphadenopathy with multiple pulmonary metastases. Well defined, ring enhancing lesions in bilateral parietooccipital lobes with surrounding oedema and mass effect were seen, possibly neoplastic (Figure 3).
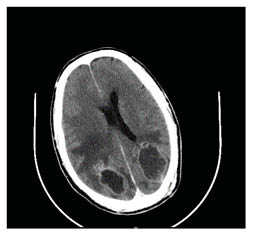
Figure 3: CT of the brain demonstrating well defined ring enhancing lesions in the parieto-occipital lobe with surrounding oedema.
In view of multiple recurrent occipital-parietal abscesses with sterile cultures (blood and drainage fluid) and the underlying lung adenocarcinoma, in consultation with the cardiologist, a possibility of marantic endocarditis was considered.
A 2D echocardiography did not show the presence of vegetations. However, increased suspicion of marantic endocarditis encouraged a further investigation and thus a transoesophageal echocardiogram was performed, which revealed vegetations on the aortic valve prolapsing into the left ventricle outflow obstruction (4 mm). The report was suggestive of grade 1 aortic regurgitation with good left ventricular function.
The patient was treated with anticoagulants for the marantic endocarditis and chemotherapy for the lung adenocarcinoma. The patient was discharged in a clinically and haemodynamically stable state.
DISCUSSION
NBTE refers to vegetations on the cardiac valve composed of thrombin and platelets. The age group most commonly susceptible to NBTE is 40–80 years.9 The clinical manifestations can be quite ambiguous; moreover, the initial manifestations are usually embolic manifestations such as focal neurological deficits, myocardial infarction, etc. However, a triad could aid in the diagnosis of NBTE, including underlying disease processes associated with NBTE such as connective diseases, malignancies, etc.; new onset of heart murmur; and evidence of multiple systemic emboli.10
In patients presenting with an embolus, the commonly involved arteries include cerebral, coronary, renal, and mesenteric arteries. Systemic emboli are evidenced as the primary presenting complaint in up to 50% of the cases of NBTE.5,10 However, the authors’ case presented with metastasis from a primary lung cancer, an atypical manifestation of marantic endocarditis.
Chest X-ray is the initial modality of investigation and further imaging studies are necessary if the following features are detected: bulky mediastinal lymphadenopathy or bony lesions, as this has a low sensitivity.11 A HRCT scan can identify lesions that are small, guide the placement of a needle for a lung biopsy, and guide the staging of lung cancer as well.12 In concordance with the authors’ case, the hilar lymphadenopathy showed on chest X-ray was recognised on HRCT, which revealed a comparatively comprehensive description of the adenocarcinoma.
Biopsy of the lung can be done to further confirm the diagnosis of adenocarcinoma. Up to 95% of malignant lesions and 91% of benign lesions can be detected by a transthoracic lung biopsy.13 The use of a CT-guided lung biopsy further strengthened the authors’ suspicion of lung adenocarcinoma as the possible cause of the marantic endocarditis. A few other differentials include secondaries from the lung adenocarcinoma, fungal abscess, and embolic event disseminating from the cardiac valves.
Further scrutiny by chest X-ray, CT scan, and additional lung biopsy revealed lung adenocarcinoma, which could be an inciting factor for the development of marantic endocarditis (Figure 4). This is demonstrated by the release of tissue factors in mucinous cancers such as adenocarcinoma of the lung, ovary, etc.14
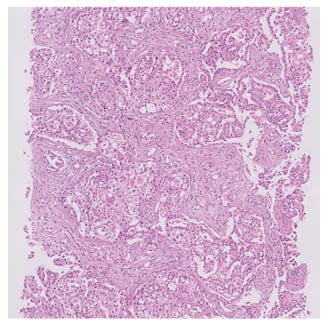
Figure 4: Lung biopsy showing adenocarcinoma
The reported cumulative incidence of brain metastasis was 16.3% in patients with lung cancer after a 5-year period in a cohort of patients with melanoma, colorectal cancer, lung adenocarcinoma, and renal carcinoma in a study conducted with a sample size of 2,724, 232 (8.5%) of whom were found to have brain metastasis. There was also an increased frequency of detection of brain metastasis with lung cancer compared to other primary tumours.15 As reported in the literature, the authors’ case also had recurrent lesions in the brain, possibly due to metastasis from the lung cancer, as suggested by the findings on the CT scan of the brain.
Transoesophageal echocardiography (TEE) has been more sensitive and specific in the diagnosis of NBTE,5 particularly if the lesions are small (less than 5 mm) and irregular in shape compared to TTE. A study of 200 patients demonstrated the involvement of left sided heart valves, particularly the mitral and aortic valves in NBTE. Of the 200 patients studied, 19% had well established vegetations and, of this 19%, 19 patients had vegetations in the mitral valve compared to 18 patients who had vegetations in the aortic valves. Furthermore, valvular lesions were found in 28% of those with carcinoma of the lung.16 The formation of vegetations in case of NBTE is quite rare as the damage that occurs is very superficial and may not be visible on TTE.9 As seen in the authors’ case, the vegetations unperceived by TTE were detected by TEE as a small vegetation on the aortic valve, emphasising the increased sensitivity of TEE.
Cytokines such as IL-1 and TNF found circulating in the blood stream of these patients further contributes to the damage to the valve, contributing to the vegetations on the valve.14 Another possible inciting factor in the authors’ case could be the COVID-19 positive status, well investigated for its hypercoagulability, which could possibly also explain the valvular damage, endothelial damage, activation of the coagulation cascade, and deposition of fibrin on the valves.17 The authors postulate that the vegetations that formed on the cardiac valve could be attributed to the above explanations.
Marantic endocarditis being onerous, probably due to its association with cancer, it preliminarily requires a high degree of suspicion followed by treatment of the underlying cause of the condition. Marantic endocarditis is composed of fibrin and platelets and therefore requires treatment with anticoagulation. Most commonly used anticoagulants in the treatment of such cases are the activators of antithrombin (i.e., heparin, particularly low molecular weight heparin). The role of warfarin in patients with NBTE has not demonstrated efficacy due to its increased risk of thromboembolism. Anticoagulants in NBTE are continued indefinitely provided there are no contra-indications. Newer anticoagulants such as factor Xa inhibitors can also be used.11,18 The authors’ case was treated with low molecular weight heparin.
To the authors’ knowledge, the essence of this case lies in the presenting neurological complaint, which was later found to be a secondary/metastasis from a primary lung adenocarcinoma, associated with marantic endocarditis.
Future prospective studies to determine the incidence and pathophysiology of marantic endocarditis presenting with metastasis are needed. Imaging studies on lesions in the brain could be done to fathom the various presentations in marantic endocarditis.
CONCLUSION
The presented case has its uniqueness in terms of presentation in the form of a neurological manifestation due to a metastasis from a lung adenocarcinoma. Thus, an extensive workup of the case of a pre-eminent neurological complaint uncovers a possible differential of an underlying process such as cancer, with a high degree of suspicion for marantic endocarditis, given the background of sterile cultures.







