BACKGROUND
Burnout is widespread in medicine, with up to 60% of oncologists and 20% of oncology fellows in the USA reporting burnout.1 Currently, there are no systematic ways to address this issue in hematology/oncology (HO) fellowship programs. In contrast to burnout, professional fulfillment is defined as happiness or meaningfulness, self-worth, self-efficacy, and satisfaction at work.2 The authors implemented a longitudinal curriculum addressing professional fulfillment in their HO fellowship program.
METHODS
Interventions to address wellness were initiated in the authors’ HO fellowship program, in the academic year (AY) 2022–2023, based on a needs assessment, including faculty-led sessions, fellow debrief sessions, and team-building activities.3 In AY 2023–2024, a new baseline needs assessment was distributed to fellows to determine topics of interest for developing a fellowship retreat and discussion throughout the year. This assessment also included three validated surveys: the Mini ReZ survey to evaluate the learning environment,4 the Patient Health Questionnaire 2 (PHQ2) to assess for depressed mood,5 and the Generalized Self-Efficacy Scale.6 Surveys were completed anonymously in person and online, and were done in July 2023, September 2023, January 2024, and February 2024. An end-of-the-year focus group was held with fellows for summative feedback. T-test and Chi-square test were used for statistical analysis.
RESULTS
Twenty-two out of 27 fellows (81.5%) completed the baseline assessment in July 2023. Topics of interest included ‘professional boundary setting’ and ‘sharing concerns and success’. Day-long, off-site fellowship retreats were designed to address the topics identified in the needs assessment, and divided into senior and first-year fellow retreats. The retreat agenda included session such as a ‘Leader’s Summit’, in which fellows visually depicted obstacles to overcome; ‘The Boundaries We Choose’, in which fellows discussed how to define boundaries in work; ‘Communicating for Improved Outcomes’, in which fellows did an exercise in active listening; and ‘Envisioning the Future’, in which fellows created vision boards of what they hoped their futures would look like. Of the 27 fellows who attended the retreats, 22 responded to post-retreat surveys, with 21 of 22 fellows indicating they found the retreat helpful (95.4%). Beyond the retreat, four didactic sessions were implemented during the AY, focusing on ‘Grief and Awe’, which included writing reflections on the topics ‘Shame Resilience’, in which fellows discussed shame in medicine; ‘Truth Rounds’, in which senior faculty shared struggles in their careers and how they overcame them; and ‘Conflict Styles’, in which fellows self-assessed their approach to conflict. A focus group at the end-of-the-year attended by 10 fellows revealed that the curriculum was well-received, with representative quotes listed in Table 1. The Mini ReZ, General Efficacy, and PHQ2 survey scores did not significantly change throughout the year.
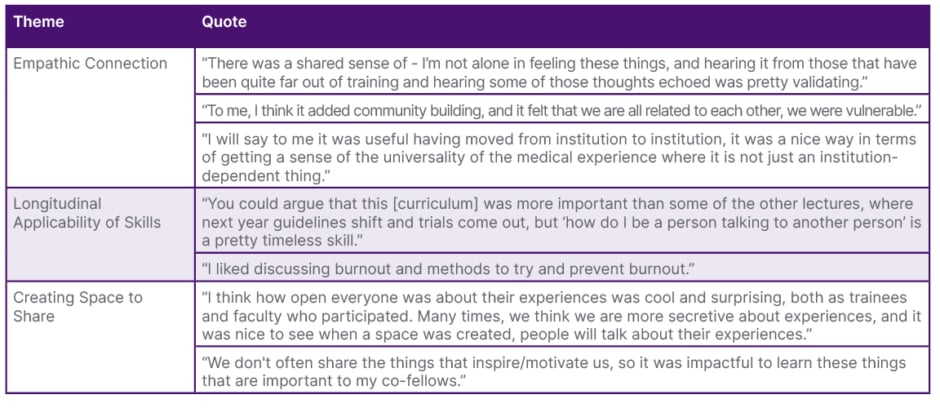
Table 1: Themes identified by fellows regarding the professional fulfillment curriculum.
CONCLUSIONS
The development of a curriculum to address professional fulfillment, including fellowship retreats that focused on topics identified by a needs assessment, was found to be helpful among HO fellows. Objective assessments evaluating learning environment and self-efficacy did not change throughout the year, and additional surveys will be obtained to measure the ongoing effect of the curriculum. This curriculum could serve as a model for other programs, and be integrated into existing trainee resources to address HO fellow wellness and professional development of skills during training.







