Abstract
This narrative review examines connections between neurology, specialist palliative care, and an integrated palliative approach to care for people living with neurodegenerative conditions. To illustrate the complexities of including palliative care in the management of neurodegenerative conditions, amyotrophic lateral sclerosis (ALS) is used as a case study. Challenges to co-ordinated ALS care and smooth care transitions between multiple services and healthcare professionals are discussed, including the timing of palliative care delivery in ALS; the education and training needs of healthcare professionals; and misperceptions of palliative care held by healthcare professionals, patients, and families. The benefits of adopting an integrated palliative approach to care for patients, families, and healthcare professionals are clarified. To enhance this, a family perspective is given on experiences of ALS neurology and palliative services, the challenges they faced, and aspects of care that facilitated the patient’s preferences for the time they had left. This review concludes that a palliative approach integrated into the care plan of people with ALS from the time of diagnosis can optimise quality of life by relieving symptoms; providing emotional, psychological, and spiritual support pre-bereavement; minimising barriers to a comfortable end of life; and supporting the family post-bereavement. These outcomes can only be achieved if palliative care knowledge and expertise are extended beyond the domain of specialist palliative care services to include the full scope of health and community-based care. These challenges and potential actions are common for several neurodegenerative pathologies, and recommendations are made for enhancing the training of neurology health professionals within the wider community.
BACKGROUND
The World Health Organization (WHO) defines palliative care as “…an approach that improves the quality of life of patients and their families facing the problem associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual.”1 People living with neurodegenerative disorders receive diagnostic, therapeutic, and end-of-life care from neurology and palliative care services. While these two disciplines may seem disparate, their goals for this patient group are aligned. As the Association of British Neurologists (ABN) states, its mission is to “…improve the health and wellbeing of people with neurological disorders by advancing the knowledge and practice of neurology in the British Isles”.2 The overlapping aims of neurology and palliative care combine when teams collaborate to improve the lives and care of people with neurodegenerative conditions such as Parkinson’s disease, multiple sclerosis, Huntington’s disease, and amyotrophic lateral sclerosis (ALS).3 Even so, non-malignant diseases such as these neurodegenerative conditions are under-represented in palliative care. A recent national Australian survey found that more people with cancer (64%) had received palliative care in comparison to non-malignant illnesses (4–10%),4 echoing results of a study conducted 10 years prior.5
Although diagnostic, therapeutic, and palliative care services operate from different perspectives, there are synergistic relationships between the neurology and palliative care teams.6 This narrative review uses ALS as a case study to comprehensively explore the relationship between these disciplines.7 This style of review was selected as the optimal way to delve deeply into this issue and uncover gaps between evidence, opinion, and practice. The aims of this review were to consider how patients benefit from an integrated interdisciplinary approach and to reveal how collaboration between neurology and palliative care teams can be strengthened.
COMPLEX CARE FOR A COMPLEX DISEASE
The complexity of ALS and the subsequent impact of a diagnosis on patients and their families highlight both the interconnectedness of, and disparities between, neurological, therapeutic, and palliative care of patients throughout the disease course. As with many other neurodegenerative conditions, ALS lacks a cure or an effective disease-slowing treatment with significant benefit. Death most frequently occurs from respiratory failure 2–4 years after symptom onset, although a small proportion of patients (estimated to be around 5–10%) live for ≥10 years.8 The presentation of the disease and the speed at which it progresses varies considerably between individuals.9 Physical symptoms can include changes in mobility, limb strength, speech, voice, swallowing, and respiratory function, and many people will also experience mild changes of varying severity in behaviour, memory, and thinking skills.10-12 A minority of patients will present with frontotemporal dementia,10 with or without accompanying physical symptoms. While a small number have an inherited form of the disease,13,14 for most, the cause is unknown.
RECEIVING A DIAGNOSIS
The complexity of ALS care begins with obtaining a diagnosis, and a timely and definitive diagnosis is an ongoing concern for patients and clinicians.15 It is important for neurologists to make a definite diagnosis rather than an early but tentative diagnosis. Establishing the diagnosis with certainty often requires periods of observation of symptom development and evolution of the clinical signs. Making an ALS diagnosis too early can cause enormous anxiety for patients and families, especially if a tentative diagnosis is incorrect. On the other hand, delays in obtaining a diagnosis can put patients at risk of depression,16 unnecessary interventions such as spinal surgery,15 and unnecessary clinical consultations.15,17
COMMUNICATING THE DIAGNOSIS
Many neurologists report being uncomfortable and inadequately trained to sensitively communicate an ALS diagnosis,18 adding to patient and carer anxiety.19-21 Moreover, in a recent Australian study, nearly 40% of patients and family carers were dissatisfied with the way they received the diagnosis.19,20 Greater adherence to effective communication techniques when delivering bad news, particularly displaying empathy, may improve the way neurologists perform this difficult task. Targeted educational programmes and the development of best practice protocols may go a long way to making these improvements attainable. Additionally, the diagnosis of ALS is frequently given by a neurologist outside of a multidisciplinary clinic (MDC) environment and without the involvement of specialised ALS services. Referral to specialised ALS and palliative care services can then be delayed until after a second opinion has been received.
Once a diagnosis is obtained, the continual progression of ALS creates further challenges to the delivery of co-ordinated patient care. Issues include timely provision of treatment and equipment22 and assessment of end-of-life care in line with patients’ preferences.23 Disruptions to service delivery can lead to fragmented care and put patient quality of care and quality of life at risk; this is a frequent concern raised by patients,24 family members,25-27 and health professionals.28
MODELS OF CO-ORDINATED CARE
In response to these challenges, specialised ALS care requires co-ordinated and multifaceted service delivery to address the variability of clinical presentations and patients’ continually changing needs. The multidisciplinary model of care (i.e., teams remaining within their boundaries to work with the patient), developed to provide comprehensive and evidence-informed patient care,29,30 has evolved into an interdisciplinary model (i.e., care teams working in an interactive, co-ordinated, and coherent way to provide patient care)31 as the spectrum of care for patients with ALS has broadened.32 Furthermore, the focus of care has become more patient-centric and the team that assembles around the patient and their family to provide care may be individualised to reflect the patient’s preferences. Thus, ALS patient teams can now include clinical care from medical, nursing, and allied health professionals from neurology, palliative care, rehabilitation, gastroenterology, respiratory medicine, and psychiatry, working alongside support services such as ALS support associations,33 genetic counselling,13 and pastoral care (Figure 1). Patients and families may also access assistance from government agencies, community services, and national ALS information and support services, and patients may integrate complementary therapies, such as massage, to assist their wellbeing. Guidelines recommend that clinical care is delivered through specialised ALS MDC to ensure care is well co-ordinated between healthcare disciplines and ALS support organisations where available.29 Specialised ALS MDC have been shown to provide effective care that can prolong patient survival time.34
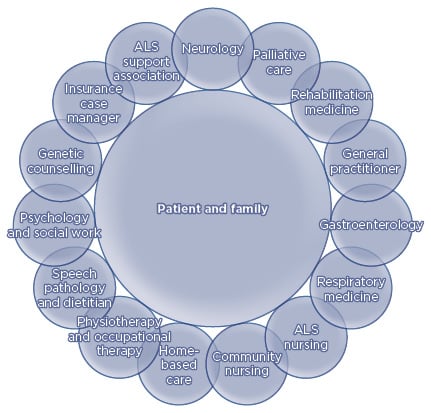
Figure 1: Interdisciplinary model of care for people living with amyotrophic lateral sclerosis.
ALS: amyotrophic lateral sclerosis.
INTEGRATING PALLIATIVE CARE INTO MULTIDISCIPLINARY CLINICS
There is increasing evidence that incorporating palliative care in MDC care, as shown in Figure 1, leads to improved symptoms and quality of life of people with ALS and their families.3,35,36 Even so, the timing of discussions of the concept of palliative care with ALS patients and when they are referred to and receive palliative care services is contentious. Introducing newly diagnosed patients to the concept of palliative care is a challenge for health professionals and can create tension between ALS therapeutic and palliative services that is often unresolved.37 Guidelines recommend that ALS patients are referred to palliative services early in the disease course to improve the patient’s quality of life,36,38,39 but patients, families, and health professionals may not be ready to discuss this type of care for some time.
Another view is that patients should be referred to palliative care once particular ALS disease milestones have been reached. However, referrals to palliative care are often triggered by crisis situations,40,41 resulting in care that is too little and too late.28 There is disparity between patient, carer, and health professional views on when and how end-of-life discussions should be conducted.42 Patients and family members may become distressed when end-of-life issues are raised,24,25 equating the topic with the end of hope. Many diagnostic and therapeutic health professionals feel unprepared to discuss end-of-life care, particularly with newly diagnosed patients.40,42 The potential consequences of avoiding palliative interventions also conflict with patient wishes for a peaceful death,43 as patients who are unable to access well-timed palliative interventions risk an uncomfortable death through poorly controlled respiratory problems, pain, and anxiety.44 The authors consider that a better way to integrate palliative care services into ALS care is to adopt a palliative approach to care, and this approach is elaborated below.
ADOPTING A PALLIATIVE APPROACH TO AMYOTROPHIC LATERAL SCLEROSIS CARE
The original intent of palliative care was as a philosophy of and approach to care; however, palliative care has now become more equated with service provision that focusses on the last months and weeks of life. A palliative approach to care begins at the time of diagnosis and does not link care provision too closely with prognosis, instead promoting early interventions for patients and their family members, aligned to their goals of care, comfort measures, and needs and wishes.45,46 The Worldwide Palliative Care Alliance (WPCA)47 has also suggested that a palliative care approach be adopted by all, not just specialist healthcare professionals, and that general palliative care be provided by primary care professionals who have an understanding of palliative care principles.
It is important to delineate the palliative care approach from specialist services since both operate at different stages of the disease trajectory. A palliative approach45 in ALS emphasises patient and family-centred care that focusses on the person and not just the disease, the importance of therapeutic relationships between care providers and the patient and their family, and clear communication throughout the illness trajectory; in particular, the approach is based on the goals of care and advance care plans (ACP) (Box 1).48
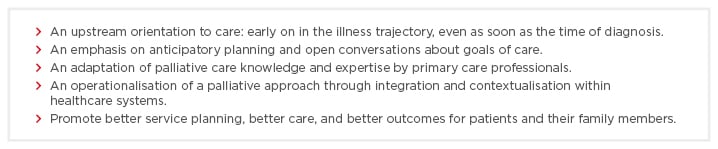
Box 1: Essential characteristics of a palliative approach.48
There is increasing evidence that a palliative approach integrated into ALS multidisciplinary care leads to improved symptoms and quality of life of people with ALS and their families.3 Integrated into the care plan for people with ALS from the time of diagnosis, a palliative approach can optimise quality of life by relieving symptoms; providing emotional, psychological, and spiritual support pre-bereavement; minimising barriers to a comfortable death; and supporting the family post-bereavement. These outcomes can only be achieved if palliative care knowledge and expertise are extended beyond the domain of specialist palliative care services to include the full scope of health and community-based care services, mostly at home, to meet the extensive range of needs of people living with ALS and their families. In most instances, a palliative approach to care can be provided in the community, supported by knowledgeable health professionals, and lasts for the duration of the disease.
Admission to a specialised palliative care inpatient facility may only occur during brief episodes of care, such as respite, symptom management, or terminal phase of illness,49 or may be required for intractable symptoms or in a crisis.45 However, the home is the preferred place of care for many patients.50,51 The palliative approach supports this by offering care delivered in the environment of the patient’s choice; control of symptoms, including medication for sleep, depression, anxiety, and distress; patient choice and control over management; holistic care; support for both the patient and their family throughout caregiving;26 and ongoing bereavement support for the family as needed.52
Barriers to Integrating a Palliative Approach
Barriers to integrating a palliative approach into ALS care arise from limited understanding of what palliative care offers, the availability of care beyond the hospice, and the effectiveness of palliative interventions for ALS.37,50 They include the belief that a palliative approach is only appropriate for end-of-life, lack of recognition that a person is terminally ill, health professionals’ lack of knowledge or interest in a new approach, discomfort with discussing the need for palliative care,45 and concern about resource and funding issues.
Overcoming these barriers involves educating health professionals, patients, and families (and the wider community) about the benefits of a palliative approach integrated into neurodegenerative disease care. As discussions about using a palliative approach can begin at any time, it can be gradually adopted so that changes to care are not abrupt. Health professionals can ensure that patients and families understand that other services, including neurology and rehabilitation, will continue alongside palliative services. In ALS, care transitions may be confusing and frightening53 because they often signal deterioration in the patient’s condition, from which there is no improvement. To fully integrate a palliative approach and to ensure transitions are seamless, education and training in integrating palliative care need to be provided to all health and community service providers involved in ALS care; education and training in the care needs of people with ALS should also be given to palliative care service providers. Educational programmes to improve the knowledge of health professionals about a palliative approach in ALS care have been recently implemented.54
Alongside a palliative approach to care, another integrated model of care for people with ALS has emerged.55 Neuropalliative rehabilitation is a speciality that recognises the intersection between neurology, rehabilitation, and palliative care services. The aims of this approach are to promote quality of life through proactive symptom management and may involve a broad range of health disciplines, such as music therapy.56 The objectives of neuropalliative rehabilitation are to prevent secondary complications, provide an environment for promoting patient health, allow treatment and modification of the disease (where possible), help the patient adapt to their altered circumstances, modify the patient’s environment to promote safety and quality of life, and support the family.55 Neuropalliative rehabilitation is particularly appropriate for people with rapidly progressive disease and those with distressing symptoms.55 While neuropalliative rehabilitation shares many of the benefits of a palliative approach, it is less easily integrated into non-specialist ALS services in the wider community, where many patients who are unable to attend MDC receive their care.
FAMILY CARERS AS PARTNERS IN A PALLIATIVE APPROACH TO AMYOTROPHIC LATERAL SCLEROSIS CARE
Family carers are vital partners in a palliative approach to care. As the patient becomes more physically dependent, family members provide logistical and hands-on care, as well as emotional support.25 A range of health professionals work closely with the patient and family to ensure effective care from diagnosis to the end of life.57 ALS service experiences of people living with ALS and their carers have provided insight into how quality of care is perceived.24,25,27,51,58 A published example from one family revealed how a palliative approach to care was perceived through the care aims, challenges, and enabling aspects encountered during their family member’s ALS journey.51 Their story, summarised in Table 1, reveals the benefits of an integrated palliative approach and how planning for a comfortable death can co-exist with living each day to the fullest.59
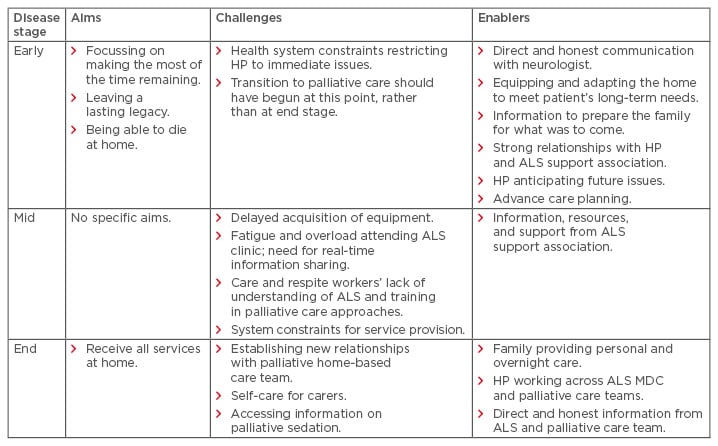
Table 1: A family’s perspectives on integrated care from diagnosis to bereavement.
ALS: amyotrophic lateral sclerosis; HP: healthcare providers; MDC: multidisciplinary clinics.
Adapted from Warren et al. in Oliver et al.59
A second example has highlighted the ongoing support and education for family carers as a further benefit of integrated approaches to care. The family, and in particular the primary family carer (most often the spouse who may act as a substitute decision maker), should be informed about all options throughout the disease course and be prepared for the impending loss of their loved one. This aims to minimise their psychological burden when they are asked to make existential decisions they are rarely well-equipped to make, and, as a consequence, reduce adverse outcomes such as complicated grief, which can continue through the bereavement stage.27,52 To this end, an Australian ALS support association has trialled the use of a person-centred international validated tool, the Carer Support Needs Assessment Tool (CSNAT), which creates the opportunity for systematically holding conversations about the practical, psychological, spiritual, and existential needs of carers in supporting their care recipients and helping themselves.60 Like the family account given in Table 1, the highest support priorities of ALS family carers were knowing what to expect in the future, knowing who to contact if concerned, equipment to help care, and dealing with feelings and worries. For the priority of knowing what to expect in the future, discussions with service providers covered end-of-life issues, advance health directives, future care, and the role of palliative care.59 This demonstrates an integrated palliative approach to care and its focus on patient and family needs.
Around the time of end of life, it is common for people with ALS to refuse life-sustaining treatment. Decisions for end-of-life care, including the use and withdrawal of ventilation and nutrition, need to be discussed with the patient and family proactively in advance of deterioration. It is important that patients and families determine their preferences and that these decisions are documented in an advance health directive or an ACP. However, the uptake of such documents is still low worldwide, ranging from 10–25%, though those who received palliative care were two to three-times more likely to have an advance health directive or ACP in place.4
Despite the inevitability of death associated with an ALS diagnosis, many families do not receive bereavement support. For example, an Australian study of ALS family carers reported that half of participants did not recall receiving offers of bereavement support and over one-third of the sample met criteria for prolonged grief disorder, a much higher proportion than the general population estimate of 10%.22 On average, palliative care services were received <2 months before patient death.22 The benefits gained by family carers in being engaged in early and direct assessment of their support needs before bereavement53 reinforce the need for palliative care services to effectively support carers well before the patient’s death.4,45 A continuum of support between caregiving and bereavement lends itself well to palliative care services that have the opportunity to investigate grief and bereavement support in the lead up to the patient’s death.4,45 This is more achievable with a palliative approach that can be initiated earlier in the disease journey, allowing a rapport to develop between the family carers and the relevant professionals within the interdisciplinary care team.
CONCLUSION
Every person with a life-limiting illness has a fundamental right to a palliative approach to care. To enable this right to be met, issues regarding palliative care, specifically equity, access, affordability, and integration in care plans, need to be considered for both current and future populations. While much research has tended to focus on specialist palliative care, there is a limit to the resources available for providing specialist palliative care to all life-limiting illnesses. Hence, the authors advocate for a more realistic palliative approach to care that is more achievable from diagnosis through to bereavement, particularly for conditions like ALS for which there is no cure or effective treatment. More improvements are still needed and these can be achieved through the strategies highlighted in this review, including those that have been trialled by ALS support associations based on research evidence. However, these can only be effective if integrated in routine practice, allowing improvements in patient and family carer outcomes and aiming for seamless patient care.
The challenges cited for ALS are common to other neurodegenerative conditions that are progressive, disabling, and lacking in curative options. Therefore, implementable actions for these conditions should target recognition of the needs of patients and their families before and after bereavement; the empathetic delivery of the diagnosis; and the essential collaboration between neurology, palliative care, primary care, and rehabilitation medicine in physical and psychological symptom management and integration of care. Generic triggers and decision points for end-of-life care include a request from the patient or their family, dysphagia, cognitive decline, dyspnoea, repeated infection, weight loss, and a marked decline in condition. Throughout this journey, open communication about disease progression, effectiveness of interventions, preparation for dying, and advance care planning should be maintained.








