BACKGROUND AND AIMS
Infective endocarditis (IE) is a common disease state observed in people who inject drugs (PWID), with a 50–100 times higher incidence in PWID than the general population.1 IE guidelines recommend valve surgery in patients who develop heart failure, have uncontrolled infection, large vegetation size, or present with systemic embolisation.2-4 However, valve surgery may not always be feasible and is infrequently performed in PWID because of the perceived risk of prosthetic valve reinfection in recidivism.1
Valve surgery in PWID remains controversial, and data are conflicting when focussed on the short and long-term benefits of valve surgery in this population.1,5-10 The timing of surgery and long-term outcomes depend on factors such as ongoing injection drug use and antimicrobial compliance;7-8 reoperation rate in PWID is significantly higher than in individuals who do not inject drugs.9-10 The objective of this study was to compare the outcomes of PWID who received valve surgery to those who did not receive
valve surgery.
MATERIALS AND METHODS
This was a retrospective cohort study performed at a large academic medical centre in southeast USA and included hospitalised PWID with IE who received and did not receive valve surgery from January 2014 to October 2018. The primary outcome was all-cause 12-month mortality; secondary outcomes included short-term mortality and infection-related readmission.
RESULTS
The study included 178 patients: 41 (23%) received valve surgery and 137 (77%) did not. Patient demographics were similar between groups, except for that patients who received valve surgery were more likely to present with septic shock (73% versus 35%; p≤0.001); 103 (58%) patients were female, and the median age was 33 (interquartile range: 27–45) years. Native-valve IE was most common in both the valve surgery and non-surgery groups (91% valve surgery versus 93% non-surgery, p=1.0), and the most frequent IE types were left-sided (54% valve surgery versus 24% non-surgery, p=0.001), right-sided (32% valve surgery versus 64% non-surgery, p=0.001), both left and right-sided (15% valve surgery versus 6% non-surgery, p=0.1), and unknown (0% valve-surgery versus 5% non-surgery, p=0.4). From 176 patients, 216 organisms were identified; the most commonly identified organisms were methicillin-resistant Staphylococcus aureus (37%), methicillin-sensitive S. aureus (25%), streptococci (9%), enterococci (9%), Pseudomonas aeruginosa (5%), Candida spp. (1%), and other organisms (23%). Patients who received valve surgery had no significant differences in in-hospital (0% versus 8%; p=0.07) and all-cause 12-month mortality (15% versus 12%; p=0.6), or all-cause 12-month readmission (54% versus 53%; p=1.0) when compared to non-surgery patients, respectively. However, patients who received valve surgery were less likely to have an infection-related readmission at 90 days compared to non-surgery patients (26% versus 72%; p≤0.001). In multivariable regression, left-sided IE was the only variable associated with all-cause 12-month mortality (Table 1).
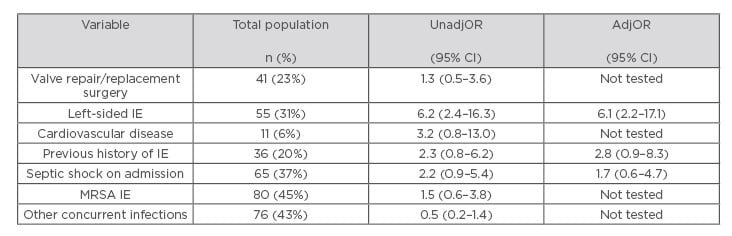
Table 1: Variables associated with all-cause 12-month mortality.
AdjOR: adjusted odds ratio; CI: confidence interval; IE: infective endocarditis; MRSA: methicillin-resistant Staphylococcus aureus; UnadjOR: unadjusted odds ratio.
DISCUSSION
Valve surgery in PWID was associated with fewer short-term infection-related readmissions but did not have any mortality benefit. These findings are significant because many previous reports showed improvement in early survival of PWID with IE after undergoing valve surgery, but subsequent poor long-term outcomes.1,7-10 Valve surgery can address the embolic and haemodynamic complications of IE, but in PWID surgery should be a part of more comprehensive management approach that includes addiction and psychiatric assessment.








