AIM
The aim of this study was to describe the prevalence of vancomycin-resistant Enterococcus faecium (VREfm)-carriers admitted to two of the hospitals in the capital region of Denmark during a 3-week screening period. The main outcome was to examine the prevalence of unknown VREfm-carriers and the secondary outcome was to compare this with the VREfm prevalence in the background population.
BACKGROUND
Vancomycin is the first-line treatment of infections caused by E. faecium. VREfm infections are increasing, especially in hospital settings. Therefore, it was of great concern when VREfm began to increase in the capital region of Denmark towards the end of 2012.1,2 Unidentified faecal carriers are a problem for infection control as they are a major reservoir of VREfm and a source for dissemination of VREfm.3 With increased numbers of VREfm-infected or colonised patients, it is evident that new measures are needed to reduce the number of VREfm cases in hospitals.
MATERIALS AND METHODS
A rectal swab was obtained from all adult patients willing to participate, who were admitted to either the emergency department at Bispebjerg Hospital or Frederiksberg Hospital during a 3-week period in June to July 2019. All patients were screened for age, hospital admissions in the last 6 months, and antibiotic treatment within the last 6 months. The swabs were analysed for VREfm by culture and PCR for the vanA and vanB genes at the Department of Clinical Microbiology, Hvidovre Hospital. The 100 faecal samples sent to the department by general practitioners in the capital region of Denmark were examined for intestinal pathogens. The exclusion criteria consisted of age <50 years, VREfm and/or Clostridioides difficile positive samples within the last 6 months, hospital admission within the last 6 months, and travel outside the Nordic countries. They were subsequently screened for VREfm as mentioned above.
RESULTS
In the study, 172 patients were included and the median age was 72 years. Within this cohort, 11 (6.3%) were colonised with VREfm, 6 (3.4%) were known VREfm-carriers, and 5 (2.9%) were unknown VREfm-carriers. Of these unknown carriers, all had been hospitalised and received antibiotics within the last month (Table 1). Of the 100 faecal swabs sent by the general practitioners, one out of 100 (1%) had positive vanA and vanB PCR and none were culture positive.
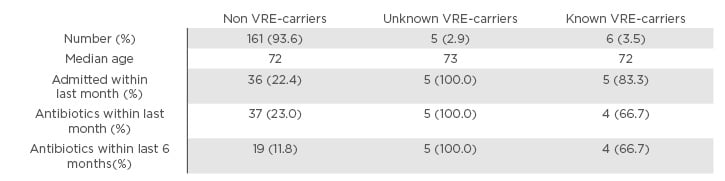
Table 1: Characteristics of the 172 patients screened during the study period.
The red circle marks the characteristics of unknown VREfm carriers.
VRE: vancomycin-resistant Enterococcus; VREfm: vancomycin-resistant Enterococcus faecium.
CONCLUSION
Hospital admission and antibiotic use within the last month predisposed to colonisation with VREfm. The authors found a prevalence of unknown VREfm-carriers of 2.9%. In comparison, 1% of the patients without prior hospitalisation or antibiotic use were VREfm positive. Admission VRE screening could help relieve the burden of VREfm transmission within hospitals. As a result of this study, the authors recommend screening all patients admitted to the emergency department who have been hospitalised within the last month.








