BACKGROUND AND AIMS
Asthma is a chronic inflammatory disease of the respiratory tract and a serious global medical and social problem.1 It is known that various aeroallergens play a key role in the triggering of asthma. Of special interest are thermo-tolerant fungi of the genus Aspergillus, which are able to reach the lower respiratory tract due to the small size of the spores. According to many authors, fungal sensitisation is associated with severe asthma course.2,3 Several studies have shown that sensitisation to one or more fungal allergens is associated with lower lung function and higher incidence of exacerbations and hospitalisations.4-6 Further characterisation of the phenotype of asthma with sensitisation to Aspergillus and the development of alternative therapy options are required to reduce the frequency of exacerbations and achieve better disease control.
The aim of the study was to assess the clinical and immunological characteristics of patients with severe asthma with Aspergillus sensitisation.
MATERIALS AND METHODS
The prospective study included 93 adult patients with severe asthma (four to five steps of therapy according to GINA 2021), with a median age of 52 years (males: 24).
The levels of thymus and activation regulated chemokine (R&D Systems, Minneapolis, Minnesota, USA), total IgE (Polignost, Saint Petersburg, Russia), and specific IgE (Alkor Bio, Saint Petersburg, Russia) to 10 allergens were determined in the blood serum by the enzyme immunoassay. Basophil activation test (BAT) with Aspergillus fumigatus allergen was performed in vitro using flow cytometry (Allergenicity kit; Beckman Coulter, Brea, California, USA). Basophils were identified by CD3–CRTH2+ marker and basophil activation by elevated expression of CD203c. The ISHAM 2013 criteria were used for Aspergillus sensitisation.7
RESULTS
Sensitisation to Aspergillus was detected in 35.4% patients with severe asthma. In the group of patients with Aspergillus sensitisation, the authors noted a lower score on the ACT questionnaire of 11.0 (10.0–16.0) versus 18.5 (13.5–21.0; p=0.000), lower FEV1 scores (57.0% [46.0–63.0] versus 72.5% [3.0–84.5]; p=0.001), and the FEV1/FVC ratio (68.0 [56.0-61.0] versus 73.7 [63.8–81.5]; p=0.025). Also, in patients with asthma with Aspergillus sensitisation, systemic corticosteroids were more often used to relieve severe exacerbations (36.4% versus 16.7%; p=0.043).
In patients with asthma with Aspergillus sensitisation, the number of basophils activated by the A. fumigatus allergen and the stimulation index (SI) were significantly higher (9.9% [6.0–24.0] versus 3.6% [2.0–5.4], p=0.000; and 4.25% [2.49–9.30] versus 0.94% [0.75–1.1], p=0.000). Significant differences in the TARC content was obtained in patients with asthma with Aspergillus sensitisation (625.0 [418.4–875.0] pg/mL versus 406.0 [210.0–561.0] pg/mL; p=0.001). The revealed significant differences in the immunological characteristics of patients with severe asthma with sensitisation to Aspergillus and without sensitisation to Aspergillus are shown in Figure 1[/hl,].
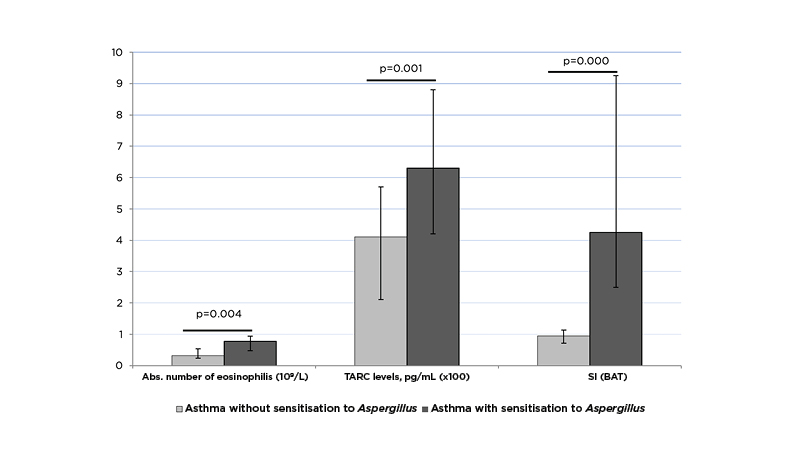
Figure 1: Immunological characteristics of patients with severe asthma with and without sensitisation to Aspergillus.
BAT: basophil activation test; SI: stimulation index; TARC: thymus and activation regulated chemokine.
A negative correlation was found between TARC levels and a decrease in FEV1 (r=-0.70; p<0.05) and positive correlation with the absolute number of eosinophils (r=0.81; p<0.05) and sIgE level to Aspergillus (r=0.36; p<0.05).
CONCLUSIONS
The study revealed clinical and functional features of asthma with sensitisation to Aspergillus spp. as a separate phenotype of a disease with a more severe course and poor prognosis. The basophil activation test is an additional method for diagnosing Aspergillus sensitisation. The TARC concentration can serve as a biomarker of an active inflammatory response.








