BACKGROUND AND AIMS
There is limited evidence to guide duration of antibiotic prophylaxis in cardiovascular surgeries. While available evidence and guidelines generally recommend a duration of 24–48 hours,1-4 there is limited comparative data to show whether 24-hour duration is as effective and safe as 48 hours. In November 2016, the surgical antibiotic prophylaxis (SAP) guidelines for cardiovascular surgeries at the authors’ centre were updated. The prior guidelines recommended a 48-hour SAP with the use of intravenous cefazolin as a first-line agent and vancomycin for those with either severe β-lactam allergy or those colonised with methicillin-resistant Staphylococcus aureus (MRSA). In the updated guidelines, duration of SAP was reduced from 48 to 24 hours and patients colonised with MRSA received dual cover with both vancomycin and cefazolin instead of vancomycin monotherapy.5 The authors conducted a retrospective study to review compliance to the updated guidelines and compare the incidence of surgical site infections (SSIs) pre- and post-implementation of the updated guidelines in order to evaluate the safety of the shortened SAP.
MATERIALS AND METHODS
A list of all patients undergoing cardiovascular surgery with sternotomy at the National Heart Centre between March 2016 and February 2019 was extracted from the hospital’s electronic database. Every fourth patient in the list was included in the analysis. The patients were then divided into three groups: Group 1 (prior to the implementation of updated guidelines, from March to October 2016), Group 2 (following the implementation of updated guidelines, from October 2017 to May 2018), and Group 3 (June 2018 to February 2019).
Patient demographics, MRSA colonisation status, drug allergy, antibiotic administration pre- and post-surgery, and the incidence of SSIs and corresponding culture data within 90 days of surgery were collected. Compliance to guidelines, in terms of choice, timing of administration, and duration of SAP, was assessed for all three groups. Both the incidence and microbiology of SSIs within 90 days of surgery were also evaluated.
RESULTS
A total of 509 patients were included in the study (Group 1: 149 patients; Group 2: 184 patients; and Group 3: 176 patients). Compliance to SAP and incidence of SSIs across the three groups are presented in Table 1. In general, the appropriate choice of antibiotic prophylaxis was consistently selected. SAP was administered in a timely fashion and highest rates of compliance were observed in Group 2, soon after the guidelines were implemented. With the implementation of the revised SAP, the proportion of patients on SAP for >24 hours decreased from 149 (100%) in Group 1 to 55 (29.9%) and 67 (38.1%) in Groups 2 and 3, respectively. Despite the reduction in duration of antibiotic prophylaxis from 48 hours to 24 hours, the incidence of SSIs did not increase. Among those who developed SSIs, the spectrum of causative pathogens was similar before and after implementation of the new guidelines.
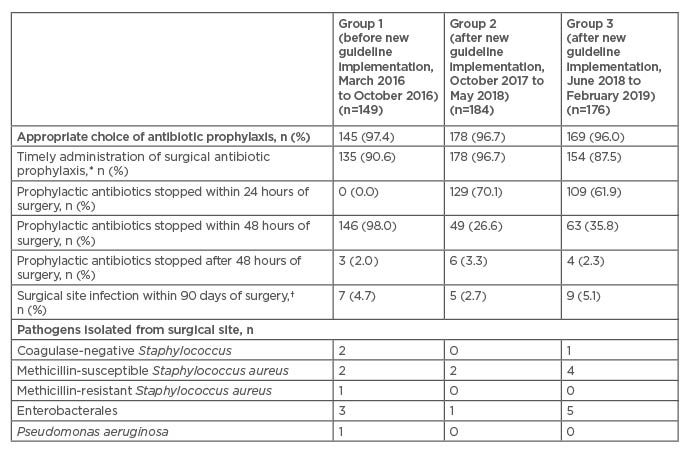
Table 1: Evaluation of compliance to surgical antibiotic prophylaxis guidelines and incidence of surgical site infections.
*This is defined as follows: cefazolin administered within 30 minutes of incision and vancomycin administered at least 1 hour prior to incision.
†Some patients had >1 microorganism isolated and, in some cases, the diagnosis of surgical site infections was made based on clinical assessment (no microorganisms were isolated).
CONCLUSION
Guideline implementation significantly reduced the duration of SAP from 48 hours to 24 hours in cardiovascular surgery at the authors’ institution, with no increase in SSI rates. The appropriate class of antibiotics was consistently selected. However, there is a role for continual feedback to ensure that SAP is administered in a timely manner and not extended unnecessarily.








