Abstract
Objective: The utility of virtual reality (VR) pain management to reduce visceral or autonomic responses is presented in 115 cases during diagnostic upper gastrointestinal (GI) endoscopy.
Methodology: 115 patients with peptic disease and gastro-oesophageal reflux were given an upper GI endoscopy with local anaesthesia. They were divided into two groups, 56 treated with VR and 59 without VR during procedures. A 10-point Visual Analogue Scale (VAS) for pain was administered to patients and the physician rated level of stress on a 3-point scale.
Results: Overall, visceral responses during oesophageal, stomach, and duodenum endoscopy were reduced using VR. Overall pain was significantly lower in the VR group than the control group with a moderate effect size. Physician stress was also reduced in the VR group, allowing greater accuracy and a shorter procedure time. A total of 115 satisfactory GI endoscopy procedures were carried out with no complications.
Conclusions: VR therapy considerably reduces the need for medication, effectively lowering costs for public health institutions and decreasing patient complications and recovery time.
INTRODUCTION
An endoscopy is an examination of the interior of a canal or hollow viscus by means of a special instrument, such as an endoscope and often calls for analgesics.1 Oesophagogastroduodenoscopy (OGD), or panendoscopy, is a diagnostic endoscopic procedure that visualises the upper part of the gastrointestinal (GI) tract up to the duodenum. OGD is also called an upper endoscopy, gastroscopy, or simply endoscopy. A gastrointestinal endoscopy aims to explore gastrointestinal structures such as the oesophagus, stomach, duodenum, biliary, and pancreatic tract. Over 1 million upper gastrointestinal endoscopies are performed each year in the USA, accounting for a significant portion of healthcare services.2 However, there are only approximately 10,000 GI physicians in the USA and that number is decreasing annually.2,3 Thus, increasing efficient and effective practices is integral to continued success and availability of GI procedures.
In the present study, we explored the oesophagus, stomach, and duodenum for diagnostic and therapeutic purposes following clinical examination and assessment. In an upper GI endoscopy there are two types of anaesthesia that may be administered to a patient depending on their preoperational condition, local anaesthesia and intravenous medication (fentanyl, midazolam).4-18 In this study, endoscopic procedures were carried out under local anaesthesia. As with many medical procedures, pain management is an essential aspect to the quality and comfort of a patient during an operation. Intravenous anaesthesia is often used to prevent pain during a procedure and reduce recall. However, with the use of local anaesthesia, a patient remains awake and cognisant of their surrounding environment, thereby enhancing their awareness of happenings and potentially increasing their risk of experiencing autonomic distress. They are however, able to co-operate during the procedure if necessary. Therefore, the introduction of pain management techniques is essential to maintaining patient comfort. Past studies and procedures underscore successful pain distraction techniques for reducing anxiety.19-27 For example, Hudson et al.22 found that when allocated distraction techniques during venous surgery, such as listening to music or watching a DVD, patients’ intraoperative anxiety ratings were significantly reduced and their overall experiences were satisfactorily improved. Additionally, Umezawa et al.23 found the application of visual distraction (watching a silent movie) worked to improve patient satisfaction and decrease both anxiety and pain while undergoing a colonoscopy. Such research highlights the successful use of pain distraction during invasive surgeries. As a result, the development and implementation of new, innovative, efficient, and effective technological pain distraction techniques is pertinent to enhancing patient comfort, reducing negative effects, and improving overall wellbeing during medical procedures.
Virtual reality (VR) as an established and effective tool in reducing autonomic response pain has been demonstrated in uterine cervical procedures (conisations, cone biopsies, etc.) and even in peritoneum manipulation in certain cases. Furthermore, VR reduces somatic pain in soft tissues of the abdominal wall, legs, arms, neck or head in outpatient surgeries. The utility of VR in decreasing pain has been demonstrated in psychology, dentistry, rehabilitation, and many other fields of medicine (Table 1).23-31 As an example, Czub and Piskorz,32 and Mühlberger et al.33 conducted studies measuring variance of pain intensity thresholds of subjects immersed in VR. Ultimately, the experiments produced higher pain thresholds for those immersed in a virtual environment. Additionally, augmented reality, a blend of physical and virtual worlds, has been applied to alleviate pain adjunctively with pharmacological analgesia in children undergoing dressing changes following burn injuries.34 In another application, Wiederhold et al.35 demonstrated the effectiveness of VR pain distraction during dental procedures. VR pain distraction has also been applied for a wide range of surgeries, including cardiac procedures.36,37 There are many applications of VR in healthcare, especially for pain management.38 Overall, the application of VR as a state management tool for medical procedures is increasingly recognised as an effective application to manage patient pain all the while costing less and being more accessible than many other analgesia options. The clinically validated capability of VR to manage pain points to a number of possible VR applications in surgery. In an attempt to expand the existing body of research, the present study explored the application of VR as an assistive anaesthetic during upper gastrointestinal endoscopy procedures. We aimed to elaborate on previous methods by examining the analgesic effects of VR in a large sample of patients. In addition, our approach to understanding the representations of pain will offer additional insight into the most effective behavioural and medical applications of VR technology.
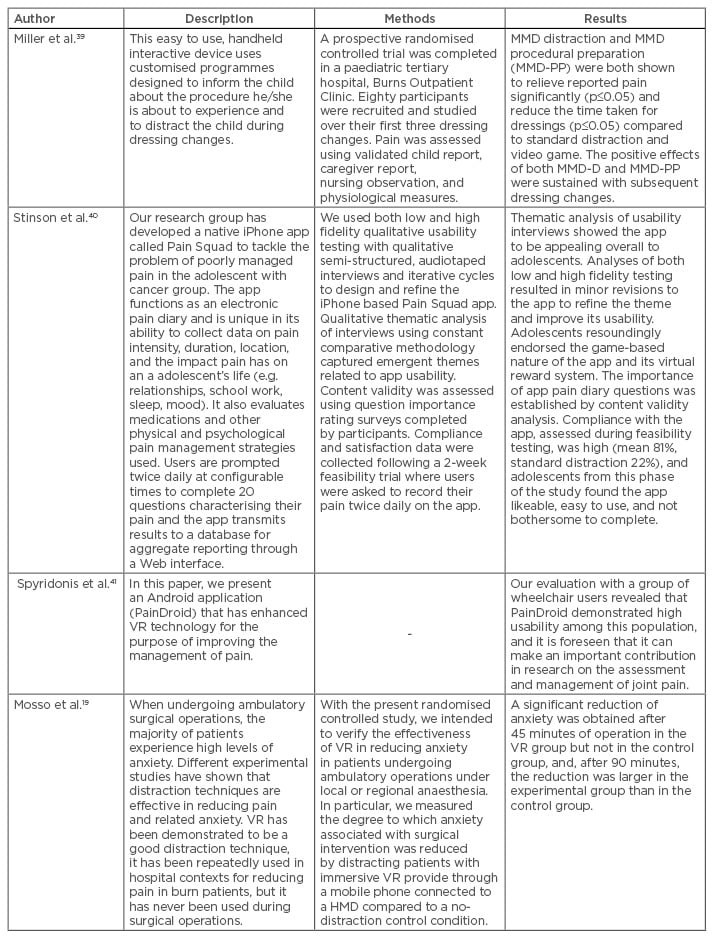
Table 1: Published studies using handheld devices in pain management.
VR: virtual reality; MMD: multi-modal distraction; MMD-PP: multi-modal distraction procedural preparation; app: application; HMD: headmounted display.
Adapted from Wiederhold et al.42
METHODS
Participants
This study took place at the Endoscopy Service at the Pisanty Clinic of the Institute for Social Security and Services for State Workers (ISSSTE) in Mexico City, Mexico. A total of 115 outpatients participated with full informed consent. There were 34 male and 81 female participants, all without cardiorespiratory disease who took part. The control group (n=59) received local anaesthesia, while the treatment group (‘VR distraction’) (n=56) received local anaesthesia and an immersive VR relaxation environment. Patients were not randomised. The average age of the control and VR groups was 53.2 and 47.6 years old, respectively. In the control group, the age range was 27–81 years (mean [M]=53.2).
Stimulus
The virtual scenarios used were: ‘Enchanted Forest’, ‘Cliff’, ‘Castle’, and ‘Beach’, all developed at the Virtual Reality Medical Center, La Jolla, San Diego, California, USA (Figure 1). Each of these four environments are clinically validated relaxation worlds to reduce autonomic stress responses and reduce pain.

Figure 1: Virtual reality headmounted display and one of four virtual environments displayed to patients.
Materials
The equipment necessary for an endoscopic procedure includes optic fibre to transmit the image to a monitor, a light source for illuminating the inside of the cavities, and insufflation to distend the virtual spaces of organs. Additionally, instruments inserted through the endoscope are used to take samples for cytological and histological examinations (biopsy forceps), and to cauterise, infiltrate, dissect, cut, and remove superficial injuries. Heart rate and additional sensors were used to measure each patient’s vitals. Gauzes were also used to measure oral secretion. We will report the findings on physiological measurement in an upcoming publication.
The VR scenarios were presented through an eMagin Headmounted Display (HMD) that displayed three-dimensional (3D) stereoscopic colour images with a resolution of 1,024×768 pixels. The auditory effects were delivered through binaural headphones. The computer was a Pentium IV, 3 GHz, 2 GB Ram, NVIDIA QuadroFX 4500 512 MB DDR3 Graphics card. Virtual scenarios were modelled and animated using 3D StudioMax, Adobe Photoshop, and Maya. Navigation was conducted with a Logitech Joypad.
Procedures
In this study, we performed diagnostic OGD and biopsies. All patients were referred to the clinic with benign diagnoses of peptic ulcer disease, gastritis, oesophageal reflux, upper bleeding, duodenogastric reflux, oesophageal varix, and human immunodeficiency virus (HIV) amongst others (Table 2). To become accustomed to the intervention, the VR group was trained how to navigate the relaxation environment prior to the procedure. Each patient’s vital signs were measured before, during, and after the endoscopy, as were their subjective perceptions of pain, measured via self-report on the Visual Analogue Scale (VAS). With the patient seated, initial vital signs and patient pain were recorded. Endoscopic procedures were done under local anaesthesia; the physician sprayed five doses of xylocaine into the oral cavity before beginning the procedure. With the patient lying on their left side decubitus with an oral protector (nozzle), the physician set up the HMD linked to a laptop in order to present one of the four virtual environments (Figure 1). The physician then inserted the endoscope through the oral cavity into the larynx. Next, the patient was instructed to swallow in order to insert the endoscope into the upper oesophagus. The VR headset and environment was then turned on and the patient began navigation. Continuing to explore the stomach and gastric antrum, the endoscopist performed a retrovision manoeuvre. The bending of an endoscope can cause pain and distention and because of this it was decided that this was the optimal time to record the in-procedure vital signs. This data was recorded as ‘face’, or pain, ‘during’. If necessary, the endoscopist took biopsy samples from the fundus, body, or antrum. We continued with the exploration of the first and second portion of duodenum where vital signs were again measured. The procedure ended and the endoscope was removed. After the endoscope was extracted, gauzes were analysed. These oral secretion measurements served as indicators of stress levels during the procedure. Patients in the VR group continued immersion in the virtual environment for 10 minutes after the conclusion of the procedure while the endoscopist cleaned the equipment. At this time, the last vital signs, pain ratings, and gauze scores were recorded.
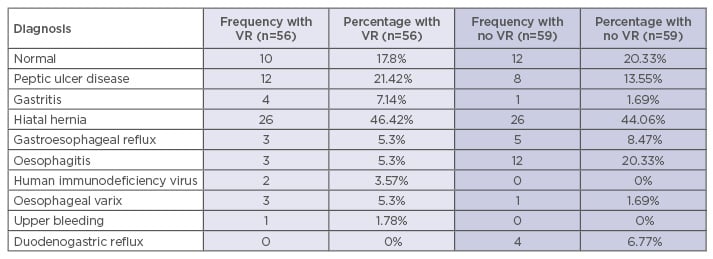
Table 2: Frequency of diagnosis: Comparison between virtual reality and control groups.
VR: virtual reality.
Measures
Subjective vital signs were recorded before, during, and after the procedure via the pain VAS. This Likert-type scale instructed patients to rate pain on a scale of 0–10 (0=no pain, 10=maximum pain). Physician stress was measured on a self-report scale of 1–3 (1=no stress, 2=some stress, 3=much stress). The length of the procedure was also recorded.
Statistical Analysis
For the assessment of differences in measurements of perceived pain between the VR and control groups, multiple one-way analyses of variance (ANOVA) were run. Cohen’s d tests were run to assess effect size. Statistical significance was set at p≤0.05. All data analysis was conducted using Microsoft Excel.
RESULTS
Table 3 presents mean values and significance levels of the differences between the VR and control group during upper gastrointestinal surgery with local anaesthesia. First, overall pain, as measured on the VAS scale (0=no pain, 10=maximum pain) was 31% lower for patients in the VR group (M=4.536, standard deviation [SD]=2.662) than the control group (M=5.814, SD=2.921), (F [1, 113]=5.991, p=0.016, d=0.469). While statistically non-significant, the average time per procedure with VR was 30% faster than without, a clinically significant difference between groups. The VR group averaged 5.17 minutes per procedure (SD=1.523) while the control group averaged 5.97 minutes per procedure (SD=3.279) and d=0.29, suggesting that VR has a small effect on reducing time per procedure (F [1, 111]=2.33, p=0.13). Comparisons of physician stress also produced clinically significant differences. The physician rated his stress level lower when operating on the VR group (M=1.43, SD=0.599) than the control (M=1.64, SD=0.689) (F [1, 113]=3.19, p=0.077 d=0.34). No complications were presented in this study.
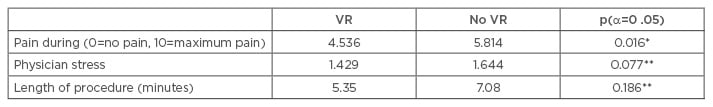
Table 3: Pain distraction during endoscopic surgery. Comparison between virtual reality and control groups on perceived pain, physician stress, and length of procedure.
*p<0.05, **clinically significant.
VR: virtual reality.
DISCUSSION
This study adds to the current body of research regarding the efficacy of immersive VR distraction for invasive medical procedures and highlights specific ways in which this technology can be successfully applied. VR was shown to reduce pain during medical procedures in this group of 115 patients. The results were statistically significant. VR has a small effect on reducing the time per procedure. In addition, analyses indicate that patient stress positively correlates with physician stress, suggesting that as a patient exhibits physiological signs of discomfort, the physician too reflects higher stress levels. Moreover, due to the moderate effect size of VR on physician stress, we suspect that VR can be an important tool to help physicians relax as well. We have shown in a number of clinical studies that levels of immersion are important for an effective VR experience. Because our VR worlds are highly engaging and interactive, patients were able to become immersed, which was supported by much lower subjective pain ratings. Overall, we conclude that the ability of the VR intervention to produce statistically significant lower levels of pain underlines its capability as an effective tool in managing physiological responses.
CONCLUSION
As virtual distraction gains traction and is used in conjunction with pharmacological analgesia, there is potential for lower costs in medication and hospitalisation. Aside from lowering costs, VR as a technique of pain distraction can lower medical risks associated with pharmacological analgesia in both public and private health institutions. VR is a non-invasive technology and has the advantage of being easy to use. With VR distraction, practitioners avoid risk factors associated with pharmacological agents such as over-sedation, hypoventilation, and vasovagal episodes. Currently, rapid technological improvements in mobile phones and other mobile devices are facilitating the replacement of bulky, hard-to-handle HMDs with low-cost, easily accessible products. VR scenarios are becoming widely available on today’s smart mobile phones and allow patients to easily navigate virtual worlds. Subsequently, the low cost of VR equipment makes it readily available to more institutions interested in using this technology for additional treatments. Overall, this study and the body of research before it contributes to the conversation about the impending ubiquity of VR and both its known and undiscovered benefits across medical settings.
Future research may complement this study by exploring, in greater depth, more reliable physiological and subjective measurements of pain. Our study reveals the effectiveness of VR pain distraction in clinical settings (i.e. the operating room) while a patient is sedated or under some form of pharmacological agent. Nonetheless, it is important that subsequent research be conducted to explore societal applications of VR as an analgesic alternative to pharmacological agents.
VR-assisted analgesia is an effective adjunct to pharmacological agents and is trending toward being a low-cost, highly effective, and widely accessible tool for pain management. Continually evolving research and development on such technologies suggests that VR holds a promising position in the future of healthcare.








