INTRODUCTION
Assessment of liver fibrosis is vital for enabling therapeutic decisions and prognostic evaluation of chronic hepatitis. The fibrosis-4 index (FIB-4) and aspartate aminotransferase (AST) to platelet ratio index (APRI) are simple, noninvasive, inexpensive scores.1
However, their accuracy is questioned because studies of the scores are based on a few hundred patients, and did not exclude decompensated cirrhosis that is easy to diagnose.1,2 The Egyptian National Committee for Control of Viral Hepatitis has provided a rich pool of electronic patients’ records with liver biopsy results.
This chance will not be repeated or available in the future, with the new era of directly acting antiviral therapy which does not necessitate liver biopsy. The authors were motivated by the opportunity to revise and validate the accuracy of FIB-4 and APRI scores, and to further explore the potential for developing an accurate prediction method using a machine learning (ML) approach.
METHODS
This retrospective, multicentre study included 69,106 Egyptian patients with hepatitis C viral infection (HCV) for interferon-based antiviral therapy from 2010–2014, where liver biopsy was mandatory for fibrosis assessment. FIB-4 and APRI scores were calculated and performance analysis of these scores was assessed and compared to the METAVIR scoring system (F0–F4) as a gold standard for liver fibrosis diagnosis. ML was used for feature selection and reduction to the most relevant attributes (CfsSubsetEval and best first).
RESULTS
In this study, 57,492 (83.2%) patients had F0–F2, and 11,615 (16.8%) patients had F3–F4 METAVIR scores. Score validation involved the evaluation of discrimination represented by the area under the curve (AUC), and calibration to assess agreement between predicted and observed risks (correctly classified). The revalidation of FIB-4 and APRI showed low accuracy and high disagreement with biopsy results, with overall AUC 0.68 and 0.58 respectively (Figure 1). FIB-4 diagnosed few cases (14%) of F3–F4 patients; the high specificity and negative predictive values of FIB-4 and APRI reflect the low prevalence of F3–F4 in the study population.
Recent guidelines recommend screening high-risk patients for liver cirrhosis. The high disagreement between APRI, FIB-4, and biopsy motivated the authors to develop a ML approach. Of 15 attributes, ML selected age >35 years, fetoprotein (AFP) >6.5, and platelet count <150,000 as the most relevant risk attributes, at these cut-off values. Any patient with one or more of these risk factors was considered as a possible F3–F4, with a classification accuracy of up to 92.0% and receiver operating characteristic (ROC) area 0.74 (Figure 1). High sensitivity ensures that high-risk F3–F4 patients will not be missed and will be assessed appropriately, and fibrosis screening will be reduced by 40%: the percentage of patients with no risk factors.
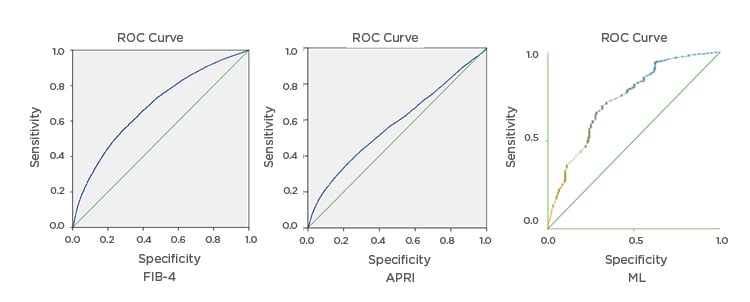
Figure 1: Receiver operating characteristic area of fibrosis-4 index (FIB-4), aspartate aminotransferase to platelet ratio index, and machine learning approach for prediction of F3-F4.
APRI: aspartate aminotransferase to platelet ratio index; FIB-4: fibrosis-4 index; ML: machine learning; ROC: receiver operating characteristic.

![EMJ Hepatology [Supplement 2] ILC Congress Review 2020](https://www.emjreviews.com/wp-content/uploads/2020/10/EMJ-Hepatology-8-Suppl-2-Feature-Image-940x572.jpg)






