India is home to approximately 100,000 people living with transfusion-dependent severe thalassaemia,1 and yet very little data on survival are available for this group of patients. Since the year 2000, oral chelators, namely deferasirox and deferiprone, have been widely available, and universal screening of blood units for HIV, hepatitis B, and hepatitis C has been mandated by the Indian government. In this era, which has opened the possibility of safer blood and access to iron chelation therapy, one would expect to see improvement in the outcomes for these patients, thereby furthering the case to have benchmarks of mortality associated with thalassaemia. A group led by the Sankalp India Foundation, Bangalore, India, has recently summarised life expectancy and risk factors of death associated with transfusion-dependent thalassaemia in 1,087 patients from 5 centres in South India from 2011 to 2018, and presented this data at the 2019 American Society of Hematology (ASH) Annual Meeting in Orlando, Florida, USA.2 The study concluded that 50% of transfusion-dependent thalassaemia patients who are receiving supportive care die by the age of 26 years old (Figure 1). A significant finding included the fact that the mortality rate of those <5 years old was also 7.0-times higher than that of the general population.
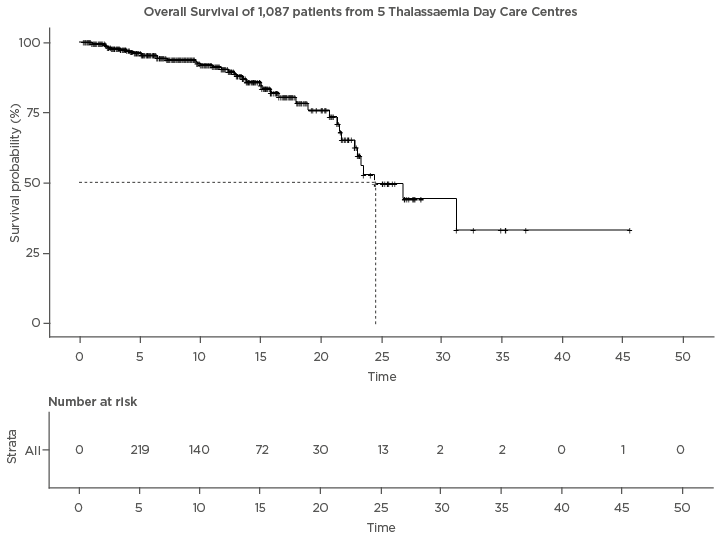
Figure 1: Kaplan-Meier survival curve.
The Cnaan and Ryan3 approach was employed, whereby patients enter and leave the study cohort and observation begins only at enrolment, and not at the onset of the disease.
The study also analysed the potential contributors to mortality. Among the factors which were reported to be significant, patients with transfusion-transmitted infections were reported to be at a 3.4-times higher risk of death. Patients who had high serum ferritin levels (>4,000 ng/dL) were at a 4.6-times higher risk of death compared to those who had serum ferritin under control (<1,000 ng/dL). Patients who had a haemoglobin drop of >2.2 gm/dL every week were at a 7.7-times higher risk of death, compared to those who dropped ≤1 gm/dL every week. The study showed no significant differences between sexes, economic status, and the distance travelled to receive care, which is consistent with previous reports.4 The study also showed that as patients received more years of proper care and management in dedicated centres, mortality rates dropped significantly.
This study offers baseline data and methodology to assess survival associated with thalassaemia based on real-world data. The findings may have major implications on care planning and delivery for thalassaemia patients, and suggests that optimising blood transfusion, intensifying chelation, and preventing transfusion-transmitted infection continue to be particularly important.
Moreover, as an increasing number of centres in India offer cure through bone marrow transplantation directly,5 it seems of paramount importance to have some objective data guiding patient and family counselling. Sustained efforts in these areas, coupled with increased prevention and access to safe bone marrow transplant, will ease the burden for both families and public healthcare.







