Abstract
Jejunal diverticula is a rare condition quoted to affect between 0.5% and 7.0% of the population. Usually, it is clinically silent and becomes symptomatic only when complications develop. Perforation of a jejunal diverticulum secondary to enterolith formation leading to generalised or localised peritonitis is extremely rare; even rarer is an isolated perforated jejunal diverticulum. Herein, the authors present a case of perforated isolated jejunal diverticula due to enterolith in a 60-year-old female patient managed by small bowel resection and primary anastomosis.
INTRODUCTION
Small bowel diverticula are sac-like pouchings of the small bowel wall that can occur throughout the small bowel. Small bowel diverticula are most often found in the duodenum, followed by jejunum and ileum. In fact, Akhrass et al.,1 in their retrospective review of 208 patients with symptomatic small bowel diverticulosis, found that diverticula were located in the duodenum in 79% of cases, in the jejunum or ileum in 18% of cases, and in all three segments in 3% of cases. The incidence of jejunoileal diverticula is variable, reported to occur in 0.5–2.3% of individuals in radiographic series and up to 7% in autopsy studies.2 Furthermore, 77% of cases demonstrate multiple, as opposed to solitary, diverticula.3 They are more commonly reported in males, with the highest incidence in the sixth and seventh decades of life.
Small bowel diverticula are usually asymptomatic, with a spectrum of presentation ranging from non-specific abdominal pain, dyspepsia, and bloating and reaching presentations with life-threatening complications. In fact, Tsiotos et al.4 analysed 112 cases of jejunoileal diverticulosis where 42% of cases were asymptomatic; in the remaining patients, symptoms of diarrhoea were reported in 58% of patients, chronic abdominal pain in 51%, and bloating in 44% of cases. Furthermore, complication rates as high as 46% for jejunal diverticulosis have been reported and are known to be fatal at times.5 Among the complications is perforation with localised or generalised peritonitis. Herein, the authors report a case of perforated isolated jejunal diverticula due to enterolith in a 60-year-old female patient, managed by small bowel resection and primary anastomosis.
CASE REPORT
This is a case of a 60-year-old female patient with previous history of laparoscopic cholecystectomy, presenting with a 2-day history of non-specific epigastric pain associated with decreased food intake. The patient denied having a fever, nausea, vomiting, obstipation, or change in bowel habits. The patient also denied weight loss and personal or family history of malignancy.
Upon arrival to the authors’ emergency department, the patient’s vitals were stable and a physical examination of the abdomen was within normal limits, with hypoactive bowel sounds and minimal tenderness upon deep palpation of the left upper and left lower quadrants. Laboratory work-up, including complete blood count, inflammatory markers (C-reactive protein), liver function tests, amylase, and lipase, and urine analysis were within normal limits. A CT scan of the abdomen and pelvis with intravenous (IV) contrast was negative for any pertinent signs except for segmental enteritis, with no evidence of bowel suffering and no signs of ischaemia.
The patient was admitted for further management of enteritis by IV hydration and IV antibiotics (ciprofloxacin and metronidazole) for 7 days in total. Two days after the admission, the patient reported acute worsening of her abdominal pain that was associated with one episode of fever of 39 °C and chills. On physical examination of her abdomen, there was diffuse four-quadrant tenderness and rebound tenderness, more so over the left side of the abdomen.
Consequently, another CT scan with IV contrast showed diffusely thickened and enhancing jejunal loops (Figure 1A). A dilated jejunal loop up to 4.5 cm filled with bezoar or enterolith (Figure 1B), significantly increased, and surrounding fat streaking were noted, in addition to free fluid in the pelvis and along the left paracolic gutter that had not been noted on the initial CT scan 2 days previously. In view of worsening pain, the new onset of fever, and the new findings on imaging despite IV antibiotics, the authors opted for a diagnostic laparoscopy.
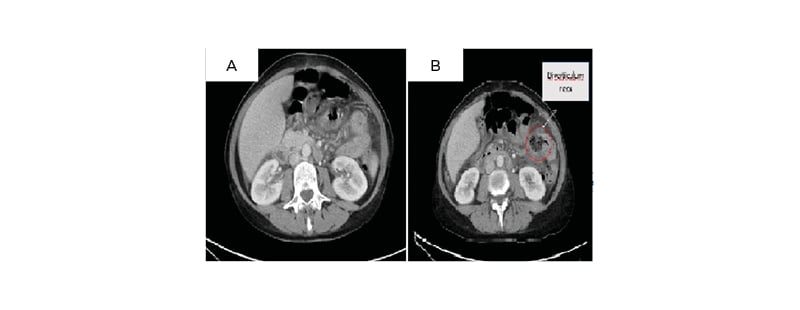
Figure 1: A) Diffuse jejunal wall thickening; and B) highlighting an enterolith or bezoar.
In the operating theatre, the patient was given general anaesthesia, a urinary Foley catheter was inserted, and the patient was placed in the modified lithotomy position. An infraumbilical incision, an open technique to access the abdominal cavity, insufflation, and the insertion of two 5 mm trocars were performed under direct vision in the suprapubic and left lower quadrant area. Sharp lysis of adhesions was done up until reaching the area of inflammation, whereby it was dissected using blunt dissection. A large jejunal diverticula on the mesenteric border measuring approximately 7 cm in diameter was identified, located 40 cm distal to the ligament of Treitz. Further blunt dissection of the diverticula from the jejunal mesentery identified an enterolith (Figure 2A). Furthermore, a jejunal perforation measuring approximately 3 cm was identified (Figure 2B). This was followed by a left paramedian 5 cm incision and placement of Alexis retractor. A small bowel segment was exteriorised and segmental resection with primary side-to-side anastomosis performed, followed by closure of the mesenteric defect (Figure 2C). Running of the small bowel from the ileocaecal valve until reaching the ligament of Treitz, the authors did not identify any other diverticula and no colonic diverticula were identified intra-operatively. Final histopathology studies confirmed the diagnosis of perforated false diverticulum with signs of necrosis and gangrene at the edges of perforation (Figure 2D). The patient’s post-operative course was smooth and the patient was discharged home on Day 4 post-operation.
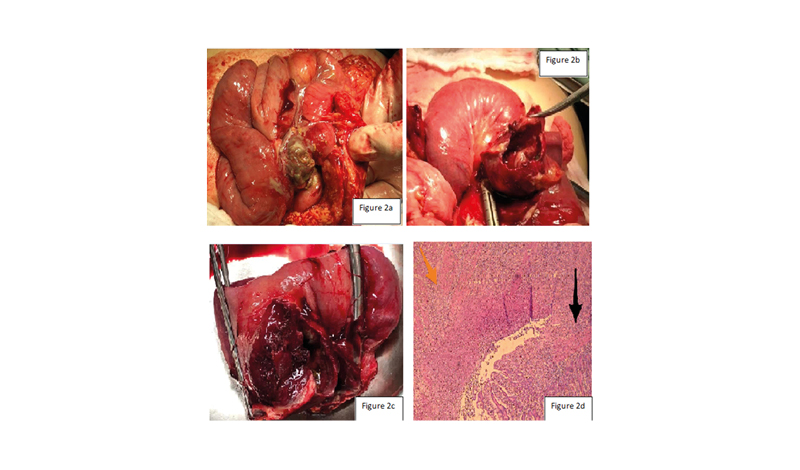
Figure 2: A) An enterolith, seen intra-operatively; B) diverticular perforation of the small bowel; C) the resected small bowel; and D) the transition from diverticular mucosa to bowel rupture, inflammation, and gangrenous formation. The black arrow represents normal mucosa while the orange arrow shows the rupture.
DISCUSSION
Small bowel diverticulosis was first reported by Sommering in 1794.6 Its aetiology is thought to be related to a combination of intestinal dyskinesia and abnormal peristalsis, causing high segmental intraluminal pressures.7 In fact, the current hypothesis focuses on abnormalities in the smooth muscle or myenteric plexus. Having said this, microscopic evaluation of jejunal specimens with diverticulosis has shown that there are three different abnormalities: fibrosis and decreased numbers of normal muscle cells, fibrosis and degenerated smooth muscle cells, and neuronal and axonal degeneration.8 The presence of any of the above-mentioned abnormalities will consequently lead to distorted smooth muscle contractions of the affected small bowel, generating areas of increased intraluminal pressure, which in turn will lead to herniation of the bowel mucosa and submucosa through the weakest point in the bowel wall, the mesenteric border at the site of entry of the vasa recta, leading to the formation of small bowel diverticula.
Small bowel diverticula are usually clinically silent and discovered incidentally or once they become complicated. However, they may have a wide spectrum of presentation, ranging from non-specific abdominal pain, dyspepsia, and bloating and reaching presentations with life-threatening complications. Life-threatening complications include massive gastrointestinal bleeding, volvulus, diverticulitis, and perforation with localised or generalised peritonitis. Furthermore, jejunal diverticulosis complicated by enteroliths is a rare entity. The enterolith, formed within small bowel diverticula, can be either de novo or secondary to a piece of undigested food. Those that form de novo are comprised of cholic acid, the end-product of bile salt metabolism, as their primary constituent. It is theorised that cholic acid enteroliths form within small bowel diverticula due to an acidic pH shift within the diverticula.9 Enterolith in jejunal diverticula can result in enterolith ileus or lead to perforation if it becomes impacted. The synergistic effect of intestinal dyskinesia with the abnormal peristalsis leads to the enterolith being stagnated due to this abnormal transit. This may eventually lead to perforation due to pressure necrosis or acute necrotising inflammation.10,11 Presentation varies widely depending on the severity of perforation. For instance, patients where the enterolith has been sitting within the diverticulum for an extended period of time, resulting in progressive erosion into the bowel wall and consequently bowel wall perforation, usually present with a localised abscess without causing the patient to become acutely ill. This is either due to the perforation into the mesentery, hence a contained perforation, or due to the walling off by the adjoining small bowel mesentery so that only localised peritonitis will occur. On the contrary, patients with acute perforation present in an acutely ill situation with gross contamination of the abdomen and generalised peritonitis. For patients with localised peritonitis and clinically stable patients, non-surgical management by IV antibiotics and CT-guided aspiration of collections may be appropriate for some patients. On the other hand, for patients with generalised peritonitis or haemodynamic instability, resection of the affected segment should be done.
Reviewing the English literature regarding perforated isolated jejunal diverticula due to enterolith has revealed only few reported cases. In fact, in the authors’ review of the medical literature, they identified a total of 23 cases of perforated jejunal diverticula (Table 1), of which five patients had isolated jejunal diverticula; their patient is the sixth reported in literature. The mean age of presentation was 71 years, with a male to female ratio of 2:1. Abdominal pain was the most frequent initial presentation.
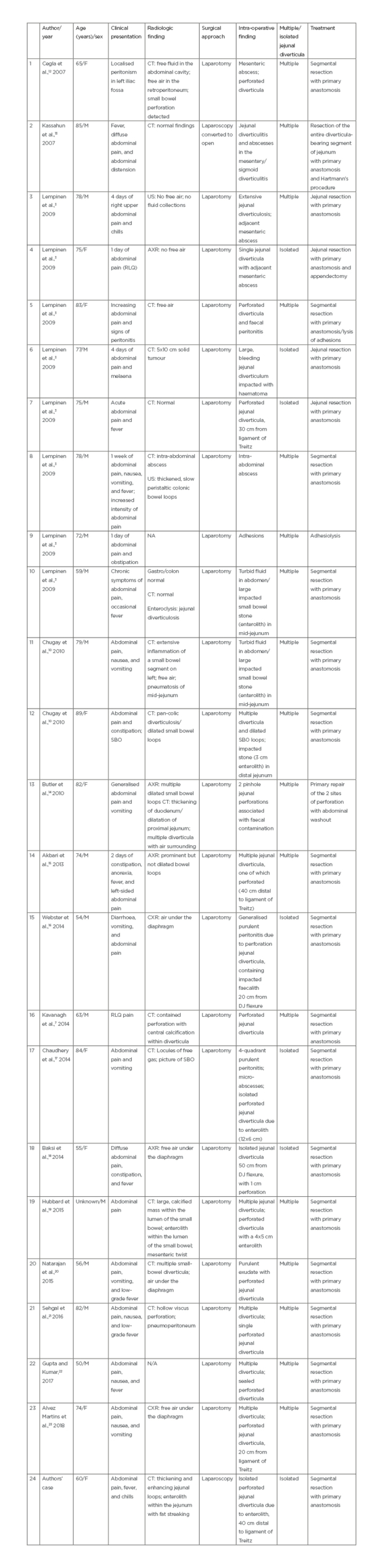
Table 1: A review of medical literature where 23 cases of perforated jejunal diverticula were identified.
AXR: abdominal x-ray; CXR: chest radiograph; DJ: duodenojejunal; F: female; M: male; N/A: not applicable; RLQ: right lower quadrant; SBO: small bowel obstruction; US: ultrasound.
All reported cases were managed surgically by laparotomy. The authors’ case was the first to utilise the laparoscopic approach and hence minimally invasive surgery in the treatment of such a rare entity. Due to its rarity, diagnosis is usually delayed. The authors’ case report highlights the importance of maintaining a high clinical suspicion of a perforated small bowel diverticulum in any patient presenting with an acute abdomen with localised signs of peritonitis. Furthermore, although non-operative management has been shown to be beneficial in stable patients, surgical exploration with segmental resection and primary anastomosis remains the mainstay of management. The authors believe that the acute onset of pain in absence of gross contamination of the abdomen was due to ischaemia, caused by the stagnated enterolith. Furthermore, the authors opted for laparoscopic approach as the patient was haemodynamically stable and this decreased the post-operative morbidity.
CONCLUSION
Jejunal diverticula is a rare entity, and their perforation is a challenge to the unaware. A delay in the diagnosis can be fatal, especially as this disease is more common in the elderly population with multiple comorbidities. Early surgical intervention when indicated is the key for successful treatment. While there is emerging evidence for the role of conservative management, the concern for progression to free perforation, especially in the setting of large, perforated diverticula, makes segmental resection the preferred intervention. Surgical approach, being laparoscopic or open, depends on the surgeon’s expertise and available resources.








