Abstract
Objective: To assess the prevalence of, and the factors associated with, contraceptive use among females living with HIV at Moi Teaching and Referral Hospital, Eldoret, Kenya.
Methods: A cross-sectional study with a sample including a total of 375 females living with HIV aged 15–49 years undergoing follow-up. Data were collected using a semi-structured questionnaire. Bivariate and multivariate analysis was done to check for association and predictors of contraceptive use.
Results: The contraceptive prevalence rate was 64%. Factors associated with contraceptive utilisation included parity (crude odds ratio [COR]: 2.33; 95% confidence interval [CI]: 1.22–4.45; P=0.010), marital status (COR: 1.75; 95% CI: 1.04–2.97; P=0.036), and availability of information on the side effects of the contraception methods (COR: 29.93; 95% CI: 14.26–70.58; P=0.001).
Multivariate analysis showed a significant association between contraceptive use and whether information on the side effects of the current contraception method was provided (adjusted OR: 34.98; 95% CI: 16.72–83.33; P=0.001).The odds of meeting the contraceptive needs of females living with HIV was 34 times higher among females who had information on side effects of the contraceptives than their counterparts who had no information.
Conclusions: The contraceptive prevalence rate was 64% among females living with HIV, higher than latest national value of 61%. Females living with HIV had a high unmet need for contraceptive use at 28.4%. Key factors associated with contraceptive utilisation included awareness of side effects.
Key Points
1. The contraceptive prevalence rate among females living with HIV at Moi Teaching and Referral Hospital, Eldoret, Kenya, was 64%, higher than the national rate of 61%; yet, there is significant unmet need for contraceptive use.2. Multivariate analysis revealed a significant association between contraceptive use, and the provision of information on the side effects of current contraception methods.
3. Counselling on the side effects of the various contraceptive methods should be emphasised, in order to empower females to make informed choices which limit discontinuation.
BACKGROUND
HIV is an epidemic in Kenya. Females living with HIV (FLHIV) have an eight-fold increased risk of a pregnancy-related death compared to females without the infection.1 This has necessitated multidisciplinary efforts in its management and control to reduce both disease progression and burden. A major weak link in this control is the prevention of mother-to-child transmission (MTCT) among infected females who are still sexually active. An estimated overall MTCT rate of 11% is very significant, and the elimination of MTCT therefore remains a key goal of Kenya’s HIV epidemic response.2
Contraceptive services for females who are HIV-positive are one of the four cornerstones of a comprehensive programme for prevention of MTCT of HIV, thereby reducing paediatric HIV infection, and are vital to meeting sexual and reproductive health needs of females who are HIV-positive.
There has been a growing trend in the contraception prevalence rate in Kenya, from 32% in 2003 to 53% in 2014, with unmet contraceptive need standing at 18% of currently married females, with 9% in need of spacing and 8% in need of limiting. A total of 31% of family planning (FP) users discontinue use of a method within 12 months of starting its use. Side effects and health concerns (11%) are the main reason for discontinuation.3
Females with unmet need are those who are fecund and sexually active, but are not using any method of contraception, and report not wanting any more children, or wanting to delay the next child.
Studies conducted on unmet contraceptive needs among FLHIV in Kenya and in Africa show mixed results, indicating differences in study settings that may influence contraceptive use. Therefore, despite the great overall progress toward increased uptake of FP, there is unmet need for consistent contraceptive use among FLHIV in Kenya.
Facilitators to contraceptive needs were not incorporated in the study of Amo-Adjei et al.,4 which the current study sought to incorporate, in addition to barriers, unmet needs, and the contraceptive prevalence rate. A review of the existing literature presented above shows that knowledge gaps exist on prevalence rate, factors associated with contraceptive use, and unmet contraceptive needs among FLHIV.
Despite pregnancy intentions being low, contraceptive use among FLHIV has been low and associated with high unmet need and consequences. However, general population contraceptive prevalence has increased, and unmet need has decreased over the last decade.3 Though a lot has been done in this field of FP and FLHIV, results have been mixed, indicating regional disparities and even disparities within countries, hence the need for local data.
In this study, the authors assess contraceptive use and factors associated with use among FLHIV in a major referral comprehensive care centre.
STUDY OBJECTIVE
The authors’ aim was to assess the prevalence and the factors associated with contraceptive use among FLHIV at Moi Teaching and Referral Hospital (MTRH), Eldoret, Kenya.
METHODOLOGY
Study Design
This was a cross-sectional study conducted at the Academic Model for Providing Access To Healthcare (AMPATH) Centre in Eldoret.
Study Population
This study targeted females between 15–49 years of age, who were living with HIV and registered at the AMPATH programme in 2019. The major role of AMPATH is to provide clinical healthcare to the general population on diseases that are affecting them, particularly targeting communicable diseases.
Sampling Procedure
Systematic sampling was adopted as the preferred sampling technique to meet the computed sample size of 377. To obtain the sampling interval (k), the calculated sample size was divided by the total population, giving a sampling interval of 18. The study sampled every 18th potential participant as per the triage register. After the first participant was recruited, there was an interval of 18 participants until the required sample size was achieved.
Data Collection Procedure and Quality Assurance
Data collection was done from the AMPATH Centre by the principal investigator and research assistants who were nurses that had been trained in data collection by the principal investigator. This was done in order to limit stigma that may arise from patients not being conversant with the investigator. Data collection was done using an electronic version of the questionnaire that was designed using EpiData Entry Software (EpiData, Odense, Denmark). Checks and balances were included in the design of the questionnaire, such that automatic pop-up alerts were activated in case wrong data were erroneously entered in a particular field. The checks also limited the participants as per the inclusion criteria, hence a candidate who did not meet the bare minimum was automatically rejected. When the last entry in the questionnaire was made, the computer prompted to save the recorded data. This limited errors associated with transfer of data during data entry.
Data Management and Analysis
The contraceptive prevalence rate among females of reproductive age living with HIV in MTRH was calculated as the percent of married females of reproductive age who were using (or whose partner was using) a contraceptive method at the time of our study. The authors included modern contraceptive methods
Inferential Analysis
A statistical model that takes into account the nominal scale of the response variable was considered for modelling the association between the dependent and independent variables. A multinomial logistic regression model was adopted as the statistical model of choice in this study. Simple and multiple forms of this model yield unadjusted and adjusted odds ratios as measure of association between the variables. The group of mothers who were not using contraceptives at all were considered as the preferred reference group for the independent variables during analysis. All the analyses were done at 95% significance level in R Studio Version 1.2.1335 statistical software (Posit, Boston, Massachusetts, USA).
Ethical Considerations
Ethical approval was sought and approved from the Institutional Research and Ethics Committee (IREC) of MTRH, and from AMPATH. Informed written consent and assent was obtained before carrying out the study from each sampled participant. Privacy and confidentiality was ensured by obtaining consent from participants in a private room.
RESULTS
Socio-demographic Characteristics of the Study Participants
In this study, the authors recruited 375 females aged 15–45 years with a mean age of 34.8 years (standard deviation: 7.5). Of these, 100 (26.7%), 153 (40.8%), 80 (21.3%), and 42 (11.2 %) participants were single, married, separated, or widowed, respectively. The majority of the study participants (334; 89.1%) had sexual partners. A total of 131 (34.9%), 13 (36.0%), and 88 (24.0%) had attained primary, secondary, and tertiary education, respectively. Moreover, 87 (23.2%), 148 (39.4%), and 138 (36.8%) participants were either employed, self-employed, or unemployed, respectively. Most participants in the study were Christians (365; 97.3%).
Contraceptive Prevalence Rate Among Females Living with HIV in MTRH
Of the 375 participants, 240 were on a modern contraceptive method, giving a contraceptive prevalence rate of 64%, while 135 (36.0%) were not using any contraceptive methods.
Male and female condoms were used by 76 (20.6%) participants, sub-dermal implants were used by 72 (19.2%) participants, while oral contraceptives were used by seven (1.8%) of the participants. A total of 68 (18.0%) participants used injections, while four (1.0%) used emergency contraceptive pills. Sterilisation was adopted by three (0.8%) of the participants, and intra-uterine devices were used by 14 (3.7%).
Sources of Information on Contraception Methods
In reference to the source from which the participants heard about contraceptives and FP, 30 (8.0%) got information from radio or television, 18 (4.8%) from newspapers, 20 (5.3%) from the internet, 321 (85.6%) from healthcare providers, and 106 (28.3%) obtained it from friends and relatives. A total of 135 (91.2%) attended antenatal care during their last pregnancy, where 124 (83.8%) said contraceptive methods were discussed.
Barriers to Contraceptive Use Among Females Living with HIV in MTRH
In total, 265 (70.7%) participants had encountered challenges in accessing contraceptives. Of those, 16 (4.3%) thought that nulliparity had partly contributed to their challenge, since they had the desire to have more children. Four (1.5%) stated that they had been denied FP access because of their age. A total of 18 (6.8%) reported that their challenge arose from their lack of knowledge on modern methods of contraception.
Side effects featured in the form of participant’s personal experiences, and what they had heard from other sources. More than half (144; 54.3%) said that the fear of side effects associated with the FP methods that they had experienced was also a contributing factor. A total of 79 (29.8%) of the participants said that what they had heard about side effects of contraceptives was a challenge, hence making it hard for them to use contraceptives.
In respect to cost, six (2.3%) and five (1.9%) of the participants cited inability to afford the cost of consultation and contraception, respectively. Couple counselling also featured as a challenge, whereby 14 (5.3%) participants reported that their husband or male partners were never involved in discussions on FP methods. Moreover, 42 (15.8 %) participants admitted that traditional beliefs in their community had prevented them from using contraceptives. The participants, however, did not specify any of the cultural beliefs (Table 1).
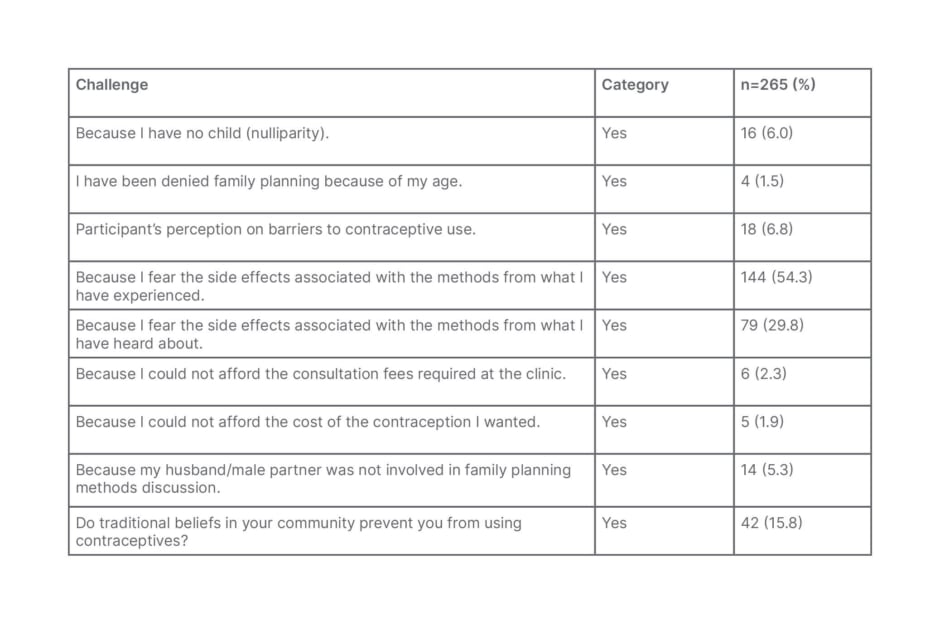
Table 1: Barriers to contraceptive use among females living with HIV in Moi Teaching and Referral Hospital, Eldoret, Kenya.
Challenges with Dual Method of Contraception
In relation to challenges, 258 (68.8%) participants acknowledged that they were facing some challenges in the use of dual methods recommended for prevention of sexually transmitted infections, while 117 (31.2%) had no challenges.
Inconsistent use of condoms was reported by 184 (49.1%) participants. This was followed closely by partner’s negative attitude towards condom use, reported by 123 (32.8%) participants.
Discontinuation
More than half (267; 71.2%) of the participants had once discontinued a contraceptive method within the first year of contraceptive use. Out of 267 participants, 118 (44.2%) reported side effects as a reason for the discontinuation. A total of 77 (28.8 %) subjects desired to get pregnant. In relation to health challenges, 32 (12.0%) participants reported that their health challenges had led to the discontinuation of contraceptive use. Method failure marked by pregnancy while on contraceptive was acknowledged by 40 out of 267 participants (15%).
Facilitators to Choice of Contraceptive Use
When asked about what could be done to improve the use of contraceptives, the study participants reported the main facilitators of FP use were increased awareness on the availability of FP methods at 99.2%, and the knowledge of the side effects of contraceptive use at 94.9%
Inferential Statistics on the Association Between Contraceptive Use and Independent Variables
Bivariate analysis showed a significant association between contraceptive use with parity (crude odds ratio [COR]: 2.33; 95% confidence interval [CI]: 1.22–4.45; p=0.010), marital status (COR: 1.75; 95% CI: 1.04–2.97; p=0.036), and availability of information on the side effects of the current contraception methods (COR: 29.93; 95% CI: 14.26–70.58; P=0.001).
Other variables, like awareness on the availability of contraceptive methods, travelling distance, transport cost, age, employment status, and education, were not significantly related to contraceptive use (Table 2).
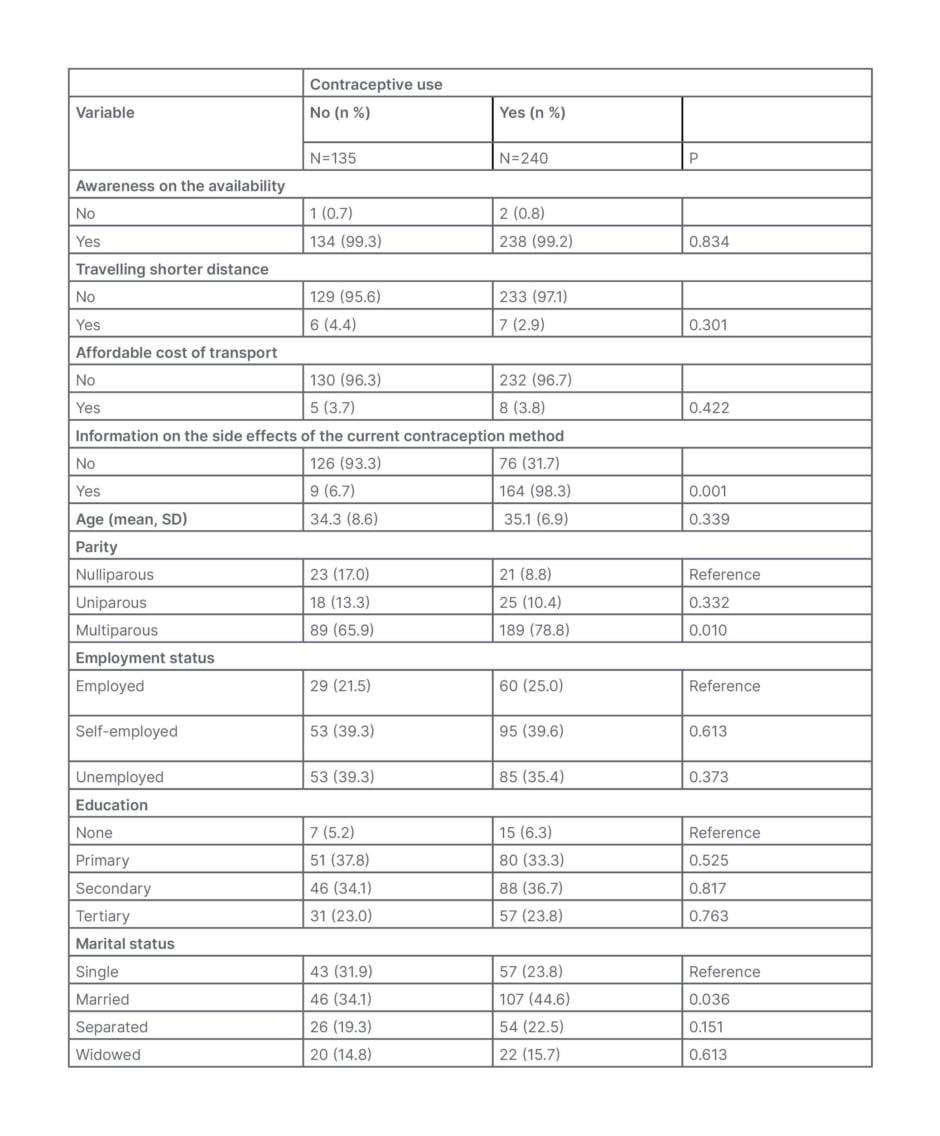
Table 2: Bivariate association between contraceptive use among females living with HIV and selected variables.
SD: standard deviation.
Multivariate analysis showed a significant association between contraceptive use and availability of information on the side effects of the contraception methods (adjusted OR: 34.98; 95% CI: 16.72–83.33; P=0.001). Parity and marital status both became non-significant in the multivariate analysis.
The odds of meeting the contraceptive needs of FLHIV was 34 times higher among females who had information on side effects of the contraceptives than their counterparts who had no information (Table 3).
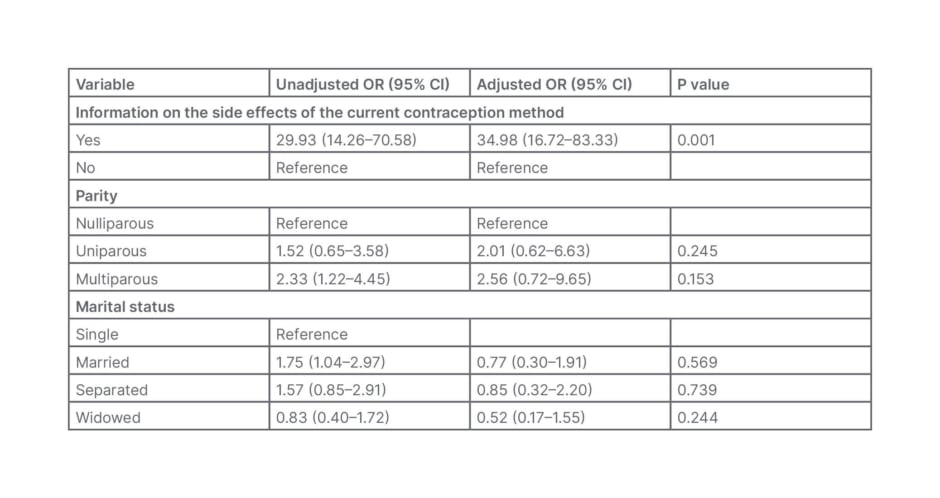
Table 3: Multivariate logistic regression after adjusting for confounding variables.
CI: confidence interval; OR: odds ratio.
DISCUSSION
Contraceptive Prevalence Rate among Females Living with HIV in MTRH
Of the 375 participants, 240 were on a modern contraceptive method, giving a contraceptive prevalence rate of 64%.
The increase in contraceptive prevalence rate that has been reported recently is probably in both FLHIV, as well as in the general population. The authors stipulate that recent efforts to integrate FP in HIV services may have resulted in better counselling, which may have resulted in increased uptake, and possibly less discontinuation rates.
In terms of popular contraceptive methods, the authors found most females were using the male condom. This is consistent with the Kenya Family Planning report 2020, which showed that condoms were the most used form of contraceptive.5
The authors results are in contrast with a study done by Mumbo et al.,6 which found the prevalence rate of contraceptive utilisation to be 79% among the study participants in a study done in Kwale, Kenya.6 Similar results were reported by Adesola et al.7 in Nigeria, who found a contraceptive prevalence rate of 67.7% among FLHIV, and Chibwesha et al.8 in Zambia, where the contraceptive prevalence rate was 69% among FLHIV.
From the bivariate analysis, there was a significant association between marital status, parity, information on the side effects of contraceptives, and contraceptive utilisation. More married females used the FP method than single females, but this was not statistically significant. This could have been caused by the sample size, and the distribution of numbers on the marital status variable.
According to the Kenya Demographic and Health Survey,3 contraceptive use was higher among sexually active, unmarried females (60.9%) than among married females (53.2%). There may be autonomy in decision-making for single females and those not in union as compared to those in a union.9
Facilitators and Barriers to Contraceptive Use Among Females Living with HIV in MTRH
Knowledge about contraceptives side effects
There was a statistically significant association with information on the side effects of the current contraception method at multivariable analysis. The odds of meeting the contraceptive needs of FLHIV was 34 times higher in females who had information on side effects of the contraceptives, compared with their counterparts who had no information. These findings compare with a study by Ryan et al.,10 which showed that knowledge of contraceptive methods was an important predictor of use, associated at logistic regression knowledge with 33% (OR: 1.33) increased odds of using contraceptives.10
The effect of counselling on contraception use is quite important in the correction of myths and misconceptions related to contraception use, creating awareness of the various contraception options for FLHIV to make their preferred choices of FP methods, and in addressing other FP related barriers.
CONCLUSIONS AND RECOMMENDATION
Conclusions
The authors found a contraceptive prevalence rate of 64%, which is higher than the latest national value of 61%, which is a good thing for this facility. The unmet need for FP for FLHIV was 28.4% higher than the African average of 24.2%. This percentage is high, and needs to be reduced by providing contraceptives and health education. Fear of the side effects was the main barrier or discontinuation factor for contraceptive use. The male condom was the most commonly used method of contraception; however, the majority also reported inconsistent use. The authors encourage the use of male condoms, since it is the most readily available means of contraception, with no known side effects.
Recommendations
The authors recommend that health professionals should encourage reproductive choices of females who are HIV-positive by increasing counselling and appropriate contraception provision at the time of HIV diagnosis, and during follow-up. Counselling on the side effects of the various contraceptive methods should be taken into account, especially at the time of giving these options, so that females are aware, and therefore make informed choice that limit discontinuation.
Study Limitations
Study limitations include that consistent and correct use in regard to the different contraceptive methods was not taken into consideration. Considering that the interviews took place at the clinic facility, there is also a possibility that the findings do not reflect what is happening at the community level.







