Words by Michaila Byrne
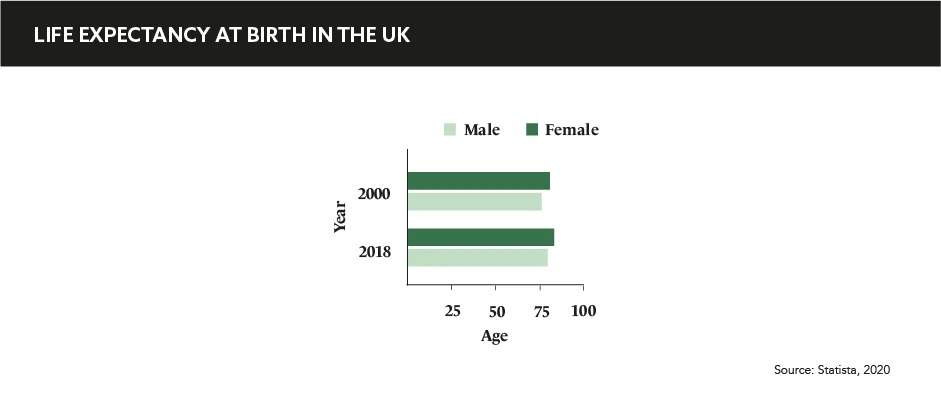
Muhammad Ali, Marlon Brando, and Achilles: all traditional archetypes of masculinity who, despite their seemingly immortal statuses, faced serious health challenges behind closed doors. In fact, across both industrialised societies and developing countries, it is men that are more burdened by illness and are dying much younger than their female counterparts. But why does this gender disparity in health exist and how can pharma better engage with male patients and encourage them to become more proactive when it comes to looking after their own health?
One flick through Men’s Health magazine and you’d be forgiven for believing that defined abdominal muscles are the sole indicator of one’s health. Such misconceptions must be challenged, and medical affairs have the power to achieve de-stigmatisation and involve men in health conversations. Suzanne Soliman, Chief Academic Officer, Accreditation Council for Medical Affairs, says: “…typically pain is the major impetus to visiting a doctor,” and as Caroline Spearpoint, Associate Director, Medical Operations & Patient Support Programs, Alexion, corroborates: “They [men] tend to hide their issues and abuse substances rather than talk about them, putting a ‘brave face’ on it.”
Although this disparity can be attributed to behavioural factors, some can also be biological, and, as Glen Poole, CEO, Australian Men’s Health Forum, suggests, even societal: “They [men] have less access to health-giving resources and greater exposure to health risks than women. This is a big challenge for healthcare providers to tackle so it’s important to focus on the areas where we can make a difference.”
They [men] have less access to health-giving resources and greater exposure to health risks than women
As healthcare partners, MA have a responsibility to recognise the multiple factors at play here, to assume responsibility for what they can impact, then subsequently act on the things that can be altered. “Unfortunately, treatment and diagnostic delay can lead to premature heart disease, later stage cancer diagnosis, and other chronic conditions which may progress beyond a point of no return,” continues Soliman. As such, it is overtly clear and vital that having men better engaged with their own health will not only benefit the health outcomes of patients in the long-term, but will facilitate earlier and more accurate diagnostics and prognoses for HCPs.
“MA has become a primary face to the medical community and therefore is a critical partner in helping improve patient care at a macroscale level through sound education and research,” says Soliman. From testicular cancer checks to addressing mental health issues, Spearpoint stipulates that campaigns like Movember, which specifically targets men, can also have a major impact on patient engagement. The earlier on a patient is engaged, the more likely they are to land within the window for actionable diagnosis.
The importance of this cannot be understated since missing that window could lead to treatment options wearing thinner and thinner: “Long term, it is about education, disease prevention, and how to spot the early warning signs. Pharma can actively consult patients via HCPs and patient advocacy organisations on the specific needs of men and how we can best support them once they’ve been diagnosed.” By actively re-focussing on this specific patient community, onboarding them at all stages of the patient journey, and accounting for their individual needs, pharma can “shift the focus from trying to make men take better care of their health, to making health services take better care of men,” says Poole.
Long term, it is about education, disease prevention, and how to spot the early warning signs
All patients desire autonomy over their life and health. Given the higher incidence rates of illness in men, MA could be key in closing this gender health gap. Health messages geared towards men have the potential to become much more nuanced and honest. If MA can appropriately engage with men in conversations about health, they can inject a sense of vigilance and pro-activity that will help men claim autonomy. Recognising that this disparity exists and can be countered by both the patient and the healthcare provider is the first step towards re-routing the conversation away from muscle mass and towards candid and accurate health management.