During the pandemic, low-to-middle-income countries (LMICs) have often been reliant on vaccine handouts from global initiatives and affluent nations. What are the emerging solutions that could improve access to vaccines in LMICs and self-sufficiency?
Words by Cheyenne Eugene
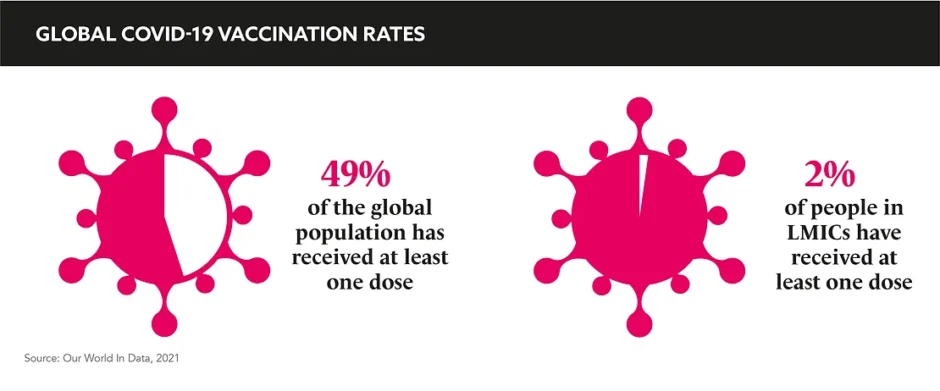
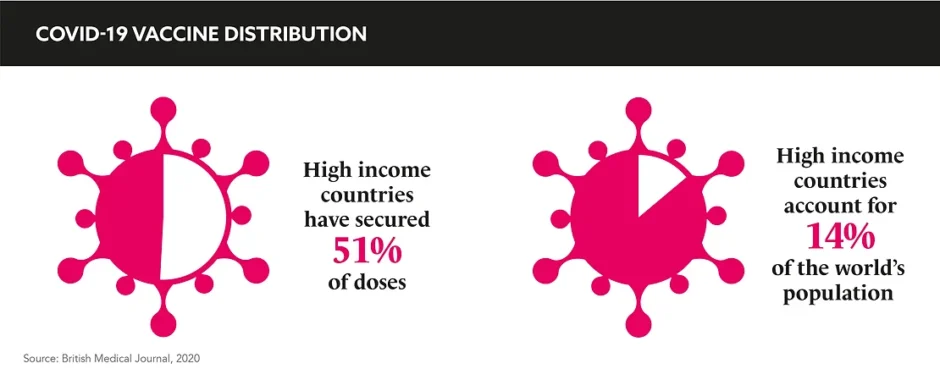
While we did not anticipate the arrival of a pandemic, global vaccine distribution is facing the challenges we expected. The richest countries have an abundance of supply, while low-to-middle-income countries (LMICs) are struggling to attain enough doses to protect themselves. In the current system, securing suitable provisions for LMICs is an elusive target, but is an opportunity for reformation on the horizon?
Dr Jack Kileba, Medical Affairs and Governance, East, West, and Central Africa, Bayer, explains how the situation unfolded: “COVID-19 vaccine development was a high-risk endeavour… The pharmaceutical industry took a big leap in advancing science and saving lives.” He continues: “Large financial investments were needed and, unfortunately, only the developed nations could afford to sign the billion-dollar upfront supply contracts which, in turn, guaranteed them preferential access to vaccines.” The consequence of this was huge inequality in vaccine access, but Kileba emphasises: “The disparity is purely financial,” and in the current arrangement, there is not much of an alternative. Seeking a silver lining, Kileba says: “One can argue that these upfront supply contracts did subsidise the development costs in favour of LMICs, but the resulting inequality is hard to ignore.”
Gaining drug access in LMICs often follows a similar route. Speaking on the EMG GOLD Podcast, Dr Jerome Kim, Director General, International Vaccine Institute, explains: “[Pharma develops the vaccine] and once pre-qualification is given, agencies like UNICEF can purchase the vaccine. And that’s how it enters the system and can be used around the world.” That’s not where the story ends: “We then actually have to create the demand for it and convince countries that there would be a cost benefit to using the vaccine.”
The disparity is purely financial
COVAX is the worldwide initiative aimed at equitable access to COVID-19 vaccines, led by a coalition of organisations – one of those being Coalition for Epidemic Preparedness Innovations (CEPI). “Ideally, it would be great to have something like CEPI for all those other diseases [affecting LMICs],” says Kim. Diseases like HIV, tuberculous, malaria, Shigella, for which no vaccine exists, kill 4-5 million people a year. “But there is no CEPI for them…There are no funders,” he highlights.
Global mechanisms like CEPI allow exact figures, strategies, and incentives to be formulated, snowballing global health action. “There was an incentive to develop COVID-19 vaccines, we knew that these vaccines would be purchased and used,” says Kim. He explains that if a vaccine’s only market exists in LMICs, who cannot financially justify the cost, the vaccine would be considered “un-incentivised”. He emphasises that this why we need an organisation that will help identify diseases of high burden and work with committed organisations to develop new vaccines.” That would be a wonderful thing,” he concludes. Kileba ponders on the idea of quotas to rebalance the scales: “I would be curious to know if the world’s trade organisations might in the future recommend quotas on essential supplies based on factors like populations at risk during the unique times of global emergencies.”
These structures would offer huge relief, but they do not necessarily build the infrastructure that empower LMICs to become self-sufficient. Local manufacturing would enhance access and embolden self-sustainability. Kileba describes the current centralised vaccine production model in large factories as, “capital intensive, inefficient, and still using very old technologies, such as the use of eggs.” He continues: “Whereas, LMICs have large and growing populations that need vaccines, but their production capacity is very low. For example, Africa produces only 10% of the vaccines it consumes.” However, Kileba goes on to explain that there is a school of thought that believes an emerging technology, known as “distributed manufacturing”, has the potential to tackle this challenge. Detailing this concept, he says: “With this, the production is done close to the final customer, and much of the material supply chain is replaced by digital information. For example, the German company, CureVac, is developing a mobile production unit that is an mRNA printer.” Models like this are ideal for LMICs where smaller factories, even mobile ones, could produce and serve the local vaccine needs.
Kim states that COVID-19 has “reminded us of the power of vaccines and vaccine development.” He says: “There’s an interest now in Europe and North America in building regional vaccine manufacturing capability in Latin America, in Africa, or additional capacity in South Asia, in order to ensure that we aren’t going to run into the situation we were in initially where all the vaccines were coming from Europe and North America, and were being used in these places first.”
Counteracting inadequate vaccine access and empowering LMICs to be self-sufficient is complex, but key themes form the basis of the solution: incentive, technology, and global partnership. With these elements considered, Kileba believes that “LMICs can move from horse and carriages to electric trains without necessarily passing through the steam engine stage.” Reforming current systems holds opportunities for pharma, in terms of investment, collaboration, and access to emerging markets. This industry is one of the loudest voices in public health and must use that to lead the global health revolution. “We need to champion,” declares Kim.