Abstract
Diabetes and stroke, with an interlinking aetiology, contribute to a growing cardiovascular disease burden and mortality around the world. Given the disproportionate prevalence and the burden of these conditions in the developing world, as well as the high risk of both Type 2 diabetes and cardiovascular disease carried by patients with metabolic syndrome, public health strategies are vital to mitigate the impact. Systematic approaches towards identifying undiagnosed patients in the community and building health systems around those targeted interventions have been implemented. However, growing evidence indicates potential for approaches to capture high-risk patients, such as those who suffer from pre-diabetes or increased insulin resistance, to provide early and optimal treatments, which could translate to population-level benefits, including reduced prevalence, disability, and disease burden.
INTRODUCTION
Cardiovascular disease (CVD), including stroke, is a leading cause of illness, death, and disability worldwide.1 A predominant factor driving morbidity and mortality is diabetes, which is a major contributor to poor outcomes in acute ischaemic stroke.2,3 Given the increasing prevalence of diabetes in the world and more specifically in Asia,4,5 it is warranted that an approach directed towards understanding the trajectories of patients with diabetes experiencing a stroke or those at a high risk of diabetes needs to be addressed. In this article, the authors discuss the emerging burden and associated morbidity of stroke in patients with diabetes and provide insights on therapeutic management from a public health perspective. The authors also provide insights on shifting the public health message towards identifying patients in the community at high risk of developing diabetes or stroke or both.
STROKE IN PATIENTS WITH DIABETES
Diabetes puts patients at higher risk for cardiovascular events, including fatal stroke, non-fatal stroke, and transient ischaemic attack.6 The clinical profile of diabetic stroke differs from a non-diabetic stroke.7 A Cochrane review showed that concurrent metabolic syndrome and diabetes were associated with recurrent strokes in patients with minor stroke and transient ischaemic attack.8,9 Furthermore, a diagnosis of diabetes is associated with an increased risk of lacunar strokes, which are associated with stroke recurrence.13 There is also evidence to suggest an increased burden of post-stroke poor clinical outcomes, such as functional disability, in patients with diabetes relative to patients without diabetes, particularly those with admission hyperglycaemia.11,12 Diabetes is associated with greater mortality, poorer neurological outcomes, poorer stroke rehabilitation outcomes, and futile recanalisation.13-17 The overall disease, financial, and social burden of stroke and diabetes is provided in Table 1.
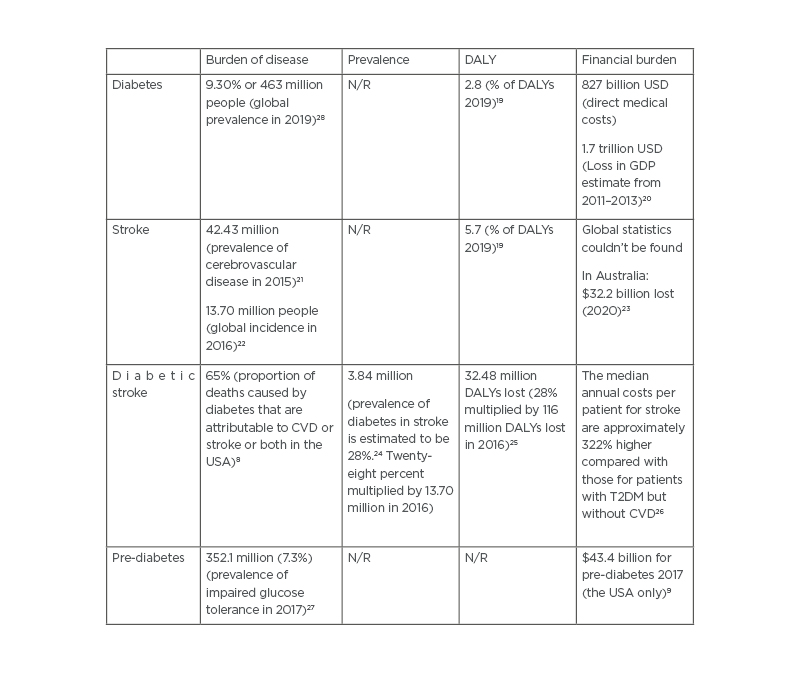
Table 1: The burden of disease, prevalence, disability-adjusted life years, and financial burden due to diabetes, stroke, diabetic stroke, and pre-diabetes.
CVD: cardiovascular disease; DALY: disability-adjusted life years; GDP: gross domestic product; N/R: not reported; T2DM: Type 2 diabetes mellitus.
It has been suggested that HbA1c levels are associated with the development of cerebral white matter damage, as higher levels of white matter damage have been seen in patients with diabetic stroke.10,28 There is conflicting evidence over whether a history of diabetes predisposes a patient to dementia, including Alzheimer’s disease.29,30 A 2016 large sample cohort study found a significant association between a history of diabetes and brain infarction, particularly lacunar strokes, with a lower mini-mental state examination (MMSE) score at the end of life, but not with Alzheimer’s disease generally.13 A novel 2021 mouse model of post-stroke cognitive impairment showed a new biomarker of brain and serum quinolinic acid concentrations and quinolinic acid-to-kynurenic acid ratios that was increased in diabetic mice.14 It was associated with long-term memory impairment, leukoaraiosis, neuronal death, and microglial and macrophage infiltration. Given the increasing burden of diabetes and global ageing populations, the impact of diabetes on cognitive function is an area of concern.
There is a lack of defined treatment protocols targeted at patients with diabetes and stroke. Given the different clinical profiles of stroke in patients with diabetes relative to patients without diabetes, there is a necessity for collaborative management between primary healthcare physicians, endocrinologists, internal medicine physicians, and neurologists. Whilst some guidelines recommend against the use of tissue plasminogen activator in patients with diabetes and previous stroke, recent evidence has shown that tissue plasminogen activator is beneficial for use in such patients.15-17 There is also a lack of consensus about the use of glucose control in stroke treatment for patients with diabetes. A 2020 meta-analysis recommended against the use of tight glucose control after ischaemic stroke because it does not improve neurological or functional outcomes but rather increases the risk of symptomatic intracranial haemorrhage and hypoglycaemia.31
PRE-DIABETES
Early identification of patients with pre-diabetes is important to reduce the burden of comorbid diabetes and stroke. A 2017 prospective cohort study compared pre-diabetes definitions that used fasting glucose (American Diabetes Association [ADA] and World Health Organization [WHO]), HbA1c (ADA and International Expert Committee [IEC]), and the 2-hour glucose tolerance test (ADA and WHO).
It found that HbA1c pre-diabetes definitions were more specific and provided a better indication of clinical complication risk.32 However, there is concern that some patients classified as pre-diabetic from glucose testing may be determined to be normoglycaemic when HbA1c alone is used, particularly patients with impaired fasting glucose.33 Furthermore, HbA1c is only an indirect measure of insulin resistance. There are also issues of availability of HbA1c testing at primary healthcare practices, particularly in certain Asian, African, and South American regions.34 Capturing at-risk individuals earlier would reduce the risk of complications associated with diabetes, and the homeostatic model assessment of insulin resistance (HOMA-IR) is a rarely used tool that can indicate insulin sensitivity and β-cell function prior to an increase in glucose levels.35
PUBLIC HEALTH APPROACHES AVAILABLE IN TARGETING THIS POPULATION
Public health approaches towards population-level screening and prevention of diabetes and stroke vary across countries. A list of public health strategies implemented in several nations is provided in Table 2.
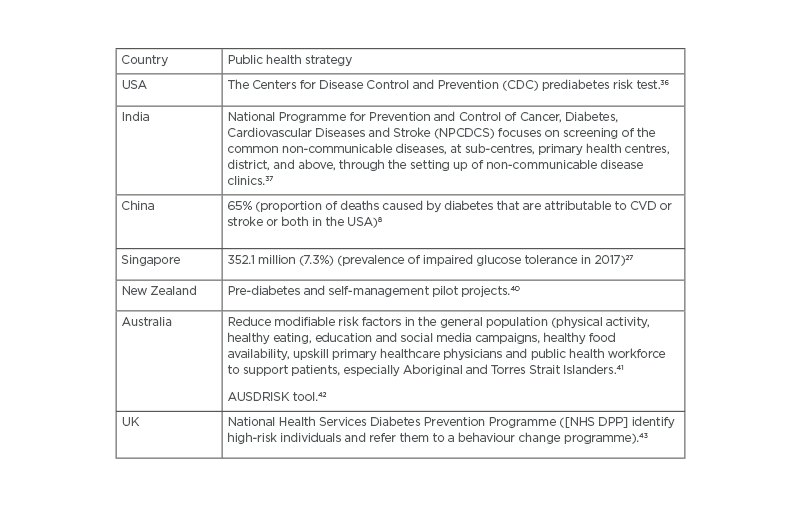
Table 2: Country-level public health strategies in diabetes screening and prevention AUSDRISK: Australian Type 2 Diabetes Risk Assessment Tool.
Role of Primary Healthcare Networks
The role of primary healthcare networks is critical in the early capture and routine monitoring of at-risk patients. Patients should receive serial glucose monitoring and should be categorised into high, moderate, and low-risk groups to determine the necessity for prophylactic anti-diabetic medication and lifestyle management. In Australia, the National Association of Diabetes Centres (NADC) network membership allows primary, secondary, and tertiary level care facilities to collaborate towards better outcomes for patients with diabetes.3 In the UK, the Diabetes UK Primary Care Network provides monthly newsletters, expert information, and resources to practitioners.4 In India, the National Programme on Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke (NPCDCS), which was launched in 2010, utilises opportunistic screening for hypertension and diabetes for persons above 30 years.37 The programme functions at all four levels of healthcare: village, sub-centre, community health centres, and district hospitals.44
Moreover, other community-led initiatives, such as a network of volunteer female community health workers, envisaged to link vulnerable individuals with the public health sector, government health initiatives, and national health programmes.18 Limited funding and underutilisation are major concerns. Mexico’s national Integrated Management of Diabetes in Stages programme at Mexico’s Institute for Social Security and Services for State Workers clinics promoted patient empowerment and education nationwide through outpatient consultations with a multidisciplinary team from 2007–2014.19 An analysis of the programme determined it to be a feasible and suitable programme to address this issue.20
Social Prescribing
Social prescribing (SP) is a method used by primary healthcare practitioners, initially implemented in the UK, that aims to connect patients with local and social services through prescription to improve patient wellbeing and health in a variety of areas.45 A review of SP practices in Bristol, UK, described three different models: SP Light, SP Medium, and SP Holistic. SP Holistic projects aim to play a preventative role and work to improve long-term conditions.46 They involve partnerships between general practitioners and tertiary care partners and sometimes evolve from SP Light and Medium models. SP Light projects aim to refer at-risk patients to specific programmes to improve outcomes, for example, prescribing exercise to a patient. In SP Medium, a health facilitator will see referred patients and provide advice on exercise, diet, programmes, and mental health support among other resources.46
An evaluation of the Community Connectors Social Prescribing Service in Bradford, UK, reported increasing coverage of the population and general practice clinics and found overall improvements of health, mental wellbeing, and social connectedness.47 An evidence synthesis of available UK studies on SP, however, found that there is not enough evidence to support the effectiveness of such programmes given the lack of uniformity in how practices implement such programmes and the need for more large-scale studies on their impact.48 SP is gaining attention internationally, and a joint report by the Royal Australian College of General Practitioners (RACGP) and the Consumers Health Forum (CHF) recommended the implementation within the Australian healthcare system to incorporate local, non-clinical services into primary care.49 Despite emerging benefits, high quality and comparable evaluations of the efficacy and cost-effectiveness of SP as a public health intervention are warranted.50
Undiagnosed Diabetes
Undiagnosed diabetes is a major problem in the community, and methods to improve asymptomatic diagnosis are needed. Epidemiological studies have demonstrated the link between insulin resistance and CVD risk, including for stroke.51,52 The landmark Insulin Resistance Intervention after Stroke (IRIS) trial showed that in insulin-resistant patients (n=3,876) without diabetes who had a recent ischaemic stroke or transient ischaemic attack, pioglitazone, a glucose-lowering drug (thiazolidinediones), reduced the risk of future vascular events, such as stroke or myocardial infarction, by 24%, and progression to diabetes by 52%, relative to those who received placebo.53 This, along with secondary analyses of IRIS data,54 highlighted the preferential use of pioglitazone in high-risk patients for stroke with Type 2 diabetes mellitus (T2DM) for primary and secondary stroke prevention.54,55 More recently, during the COVID-19 pandemic, metformin use has been associated with reduced mortality and severity in patients with T2DM.56 However, close monitoring for lactic acidosis and deterioration of kidney function is needed in patients with severe COVID-19. Moreover, population-based studies have also indicated association of increased insulin resistance, metabolic syndrome, and diabetes with increased levels of inflammatory markers, such as C-reactive protein, IL-6, and TNF-α.57,58 Use of such inflammatory biomarkers could also be considered as a useful strategy in screening patients at high risk for CVD. This is especially a problem in under-resourced settings, due to lack of access to primary care physicians, appropriate tests, and immaturity of primary healthcare networks.59,60 South Asian migrants to highly developed countries such as the UK are at a particularly high risk of CVD, due to a combination of systemic disparities and structural and innate factors. This group is a target group due to their higher risk of developing T2DM.61 Similarly, Canadian studies have shown that migrants from South Asia, Sub-Saharan Africa, Latin America, and the Caribbean have a higher burden of diabetes and CVD.62 A recent study also showed that the prevalence of undiagnosed pre-diabetes in migrant workers in Singapore increased their risk of pneumonia and electrolyte abnormalities from COVID-19.63
Recent population studies have indicated a role of retinopathy in screening high-risk individuals (e.g., those who are overweight or have elevated fasting glucose or impaired glucose tolerance) for pre-diabetes.64-67 Given the wide availability of fundus photography, as well as the ease of delineating retinal lesions, this strategy could be useful; however, this needs further validation and targeted studies in high-risk patients to warrant public health indication.68 Moreover, an important consideration is the sensitivity of the ophthalmoscopic method. This is because a prevalence of retinal lesions as high as 9.8% using 6-field fundus photography was reported in the Blue Mountain Study,69 in contrast to <1% in the Framingham Eye Study70 and Göteborg71 study in non-diabetic populations.
Community education and partnership in identifying patients at high risk of diabetes are needed, as well as awareness of diabetes in these groups. The development of targeted education modules for demonstration programmes targeted at the populations in their own languages would be beneficial. Furthermore, building the capacity of local community health workers that can teach patients about risk factors, take blood samples, participate in community-based surveillance, and utilise questionnaires to indicate symptoms-based or self-reported diabetes should be the main priority. Also, an increased awareness about post-stroke rehabilitation in patients with diabetes is needed, as these patients should be proactively educated about the risk of secondary stroke.72,73
CONCLUSION
There is an increasing need for improving surveillance of diabetes in the community and among primary healthcare networks because of the elevated risks associated with stroke in this subgroup of patients. The proposed shift towards population-based strategies (from patients with T2DM to those with pre-diabetes, metabolic syndrome, or insulin resistance), as well as using preventive measures for high-risk patients, could allow detection of those who are at increased risk of having a stroke. This approach would be helpful to improve the quality of life and reduce the burden of these chronic cardio-metabolic diseases. Furthermore, in the COVID-19 era, given the known risks of increased susceptibility to COVID-19 infections among patients with diabetes or pre-diabetes, as well as their poor clinical outcomes and increased mortality, it is imperative to explore alternative strategies to promptly identify patients at high risk, in order to maximise the opportunity to mitigate the ongoing impact of this devastating pandemic.74-76 Strategies should also focus on disproportionate burden on vulnerable communities and those from low-resource settings.75








