BACKGROUND
The idea to test the implementation of an aggressive insulin and carbohydrate intervention strategy approach to Type 1 diabetes mellitus (T1DM) athletes in a real-life trail-running endurance competition, was developed by a group of T1DM amateur athletes and members of Diabete No Limits (DNL), an Italian, nonprofit organisation, that enrolled a team of volunteers, selected by doctors, trainers, and DNL fellows, to take part in this project.
The starting points of the study were the recommendations and guidelines given to T1DM patients completing exercise, focussing almost exclusively on blood glucose (BG) levels and hypoglycaemia risk, through a conservative reduction of insulin and/or by assuming carbohydrates were consumed on a defensive eating basis. On the other hand, for non-T1DM endurance athletes a high carbohydrate supplementation strategy is strongly suggested to maximise patient response.1,2 Since the physiology of energetic substrate metabolism is the same regardless of the presence of T1DM, we asked the question: “What if a similar approach were applied to a T1DM endurance athletes?”
MATERIALS AND METHODS
In 2017, DNL enrolled eight T1DM athletes (seven males, one female), well trained in endurance sports, six receiving multiple daily dose insulin injections and two receiving continuous subcutaneous insulin infusion therapy. The mean diabetes duration in the patients was 20 years (range: 9–37 years), insulin requirements low-to-moderate (0.26–0.59; mean: 0.46 U/Kg), and good glycaemic control (HbA1c range: 6.7–7.8; mean: 7.3%).
The day before competing, the athletes completed functional tests to assess aerobic heart rate (HR); threshold and VO2 max (55–64.3; mean: 59.2), and a briefing was held focussing on metabolism, physiology, and on the scheduled collecting data protocol for the race day.
The task for athletes was to maximise running performance without reducing the insulin basal rate and boluses before, during, and after the competition, through regular supply of carbohydrates.
At the end of each lap runners had a quick stop in a dedicated transition area to check BG, lactates, HR, carbohydrate intake, and Borg scale, as well as to verify pace and lap time, to consider further carbohydrate consumption or insulin integrations, basing primarily on athlete experience and medical staff advice. Available carbohydrates were fast-acting gels, long-acting maltodextrin gels, and moderate-to-long-acting bars and isotonic beverages.
RESULTS
Bad weather conditions made the 6 km circuit, with an elevation gain of 300 m (300d+), track very tough, but all athletes completed 3–4 laps within the race limit time of 3 hours. All subjects maintained their insulin doses and carbohydrate integration ranged from 30–83 g/ hour, with 50% athletes taking >60 g/hour and the other 50% taking slightly less than that. HR was maintained in Zone 2 and 3, rising to Zone 4 occasionally for very short time periods. Lactate levels profile confirmed that energy supply was supported by aerobic metabolism (lactate peak value range: 1.7–9.6 mmol/L; mean: 3.5 mmol/L). Despite a mean carbohydrate integration of 57 g/hour, we observed a mean BG reduction of 83 mg/dL, which dropped from a mean of 201 mg/dL to 118 mg/dL, without any severe hypo or hyperglycaemic effects (range of BG: 62–242 mg/dL) (Figure 1). None of the athletes suffered nausea or gastrointestinal discomforts.
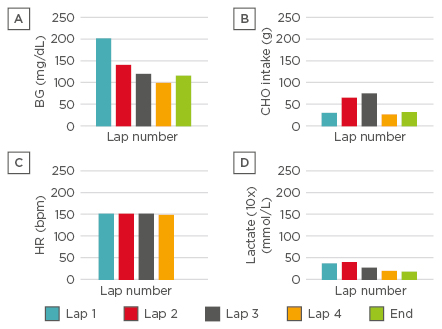
Figure 1: Mean (A) blood glucose, (B) carbohydrate intake, (C) heart rate, and (D) lactate levels measured after the completion of a 6 km endurance trail running circuit.
BG: blood glucose; CHO: carbohydrate; HR: heart rate.
CONCLUSIONS
To maximise their performance, T1DM athletes completing an endurance competition should not exclusively focus on BG levels, risk of hypo or hyperglycaemia, and ‘defensive eating-based’ carbohydrate intake. Instead, T1DM athletes should consider a ‘performance-based’ carbohydrate intake strategy. Throughout the decision-making process, balancing peculiarities of T1DM with exercise physiology, including athletic goals, duration, intensity of the effort, fitness level, and nutritional demands, must be considered.








