BACKGROUND AND AIMS
Nonalcoholic fatty liver disease (NAFLD) is the most common chronic liver disease in Western countries1 and a frequent complication of childhood obesity, with a prevalence of approximately 30% in obese youth.2,3Accumulation of intrahepatic fat has been associated with metabolic abnormalities within the liver that may directly contribute to the aetiology of Type 2 diabetes mellitus, such as reduced endogenous insulin clearance (EIC) and hepatic insulin resistance (HIRI).4-9 Differences between ethnicities in the prevalence of NAFLD, and its associated metabolic alterations, are well-documented. Compared with Caucasian backgrounds, African American people typically show reduced intrahepatic fat content (HFF).3,9Nonetheless, African American patients are also documented to have a greater prevalence of diabetes, impaired EIC, and increased HIRI.3 This paradox has led to the hypothesis of a dissociation between HFF% and liver metabolic abnormalities in populations of African ancestry.9 In this study, the authors evaluated whether, and to what extent, the HFF% contributes to impair insulin clearance and insulin sensitivity in the three most prevalent racial and ethnic groups in the USA: Caucasian, African American, and Hispanic.
MATERIALS AND METHODS
The authors analysed cross-sectional and longitudinal data from the Yale Pediatric NAFLD study,3 providing a large and well-characterised multiethnic cohort of nondiabetic adolescents who were overweight or obese (n=632). The HFF% was quantified using a validated magnitude-based MRI method.10 Insulin secretion rate, EIC, and HIRI were estimated by modelling glucose, insulin, and C-peptide data during 9-point oral glucose tolerance tests. A subgroup of subjects had repeated metabolic assessments after a median follow-up of 2 years (n=89).
RESULTS
African American individuals (27.2%; n=172) exhibited the lowest HFF% and a prevalence of NAFLD less than one-half of Caucasian individuals (36.2%; n=229) and one-third of Hispanic individuals (36.6%; n=231) (p<0.0001 for all comparisons). Furthermore, African American individuals had lower EIC (Figure 1A and 1B) and glucose stimulated ISR, but similar HIRI (Figure 1C and 1D) and plasma insulin levels. The HFF% correlated with EIC (standardised β coefficient [std. β]: -0.13, p=0.0003) and HIRI (std. β: 0.17, p<0.0001), irrespective of the ethnic background, after adjustment for age, sex, ethnicity, BMI, pubertal status, and plasma glucose levels. Consistently, EIC and HIRI declined across group-specific HFF% tertiles (Figure 1A and 1C) and were markedly lower in individuals with NAFLD (Figure 1B and 1D) in all ethnic groups. EIC and HIRI showed a negative correlation (r: -0.68, p<0.0001) that was not modulated by the ethnicity (interaction factor, p=0.69) and remained significant in adjusted models (std. β= -0.42, p<0.0001). After a 2-year observational follow up, the prevalence of adolescents whose HFF% remained stable (HFF% change ±1% or lower) was 2-fold higher in the African American group (52%) than in Caucasian (28%) and Hispanic (20%; p=0.036) individuals. Nevertheless, changes in HFF% over time were associated with changes in EIC (r: -0.25, p=0.02) and HIRI (r: 0.22, p=0.04) across all groups, without differences between ethnicities.
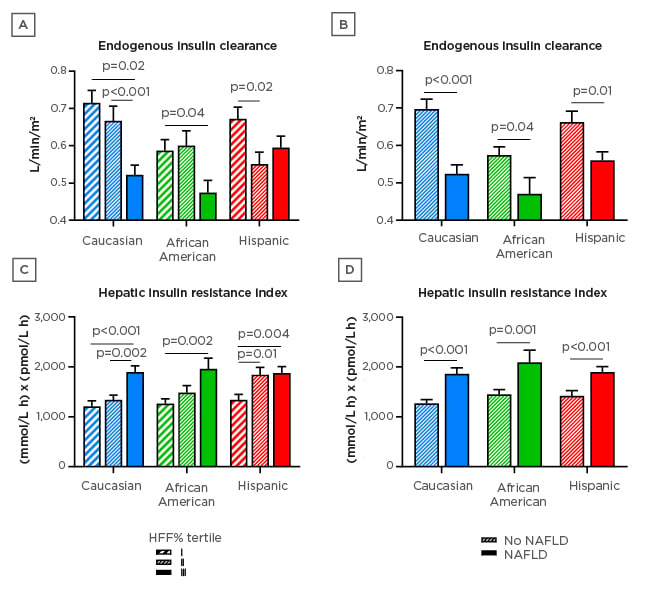
Figure 1: Hepatic fat content.
Endogenous insulin clearance by A) group-specific tertile of HFF% and B) presence of NAFLD, in obese adolescents from the Yale Pediatric NAFLD cohort. Hepatic insulin resistance index by C) group-specific HFF% tertile and D) NAFLD, in the same cohort. Data are mean ±SEM. Differences were tested by Kruskall–Wallis test followed by post hoc pairwise comparisons.
h: hour; HFF: intrahepatic fat content; NAFLD: nonalcoholic fatty liver disease; SEM: standard error of the mean.
CONCLUSION
The authors demonstrated that intrahepatic lipid accumulation is associated with reduced EIC and HIRI in obese youth, irrespective of their racial background, in cross-sectional and longitudinal analyses adjusted for multiple confounding factors. These findings support the role of fatty liver in the pathogenesis of Type 2 diabetes mellitus across different ethnicities.








