Abstract
Vitiligo is an acquired skin depigmenting disorder resulting from melanocytes loss in the epidermis, associated with an autoimmune aetiopathophysiology. However, there are limited data about the association between vitiligo and Epstein–Barr virus (EBV). Hence, the authors present a case of a 43-year-old male who had progressive symmetrical hypopigmented macules, sometimes coalescing to patches that were generalised but predominantly on the face and torso, with scanty involvement of proximal and distal extremities of the body. The diagnosis of vitiligo was made clinically, and seborrhoeic dermatitis was considered as a differential. Since the patient had been offered treatment for seborrhoeic dermatitis using antifungal with no relief and extensive depigmentation, the authors’ working diagnosis was vitiligo and was confirmed with histology. To establish the likely cause of the condition, viral serology for HIV, Cytomegalovirus, herpes, and EBV were completed, but only EBV serology was abnormal. Therefore, the authors report this case to encourage clinicians to consider EBV infection in the aetiology and predisposition for vitiligo to help explore other pathology that the virus may cause.
Key Points
1. Vitiligo is a progressive, acquired depigmenting disorder that presents through circumscribed white macules, papules, and depigmented patches in the skin. It can have significant psychological impact on affected patients.2. Aetiopathogenesis of vitiligo is multifactorial, including autoimmune disorders, which have been linked to some viral infections.
3. This case of a 43-year-old male diagnosed with vitiligo clinically and on histopathology was associated with Epstein–Barr viral infection, and 3-month treatment addressed both the vitiligo (psoralen and ultraviolet A, melatonin, and topical steroids) and the EBV infection (valaciclovir, spironolactone, and ivermectin).
CASE REPORT
A 43-year-old male from Nigeria had progressively symmetrical hypopigmented macules, sometimes coalescing to patches, which were prominent in the face, forehead, trunk, and back. On physical examination, the lesion was generalised, but the facial manifestation was of the utmost concern to the patient. There were lesions in the torso with scanty involvement of proximal and distal extremities of the body (Figure 1).
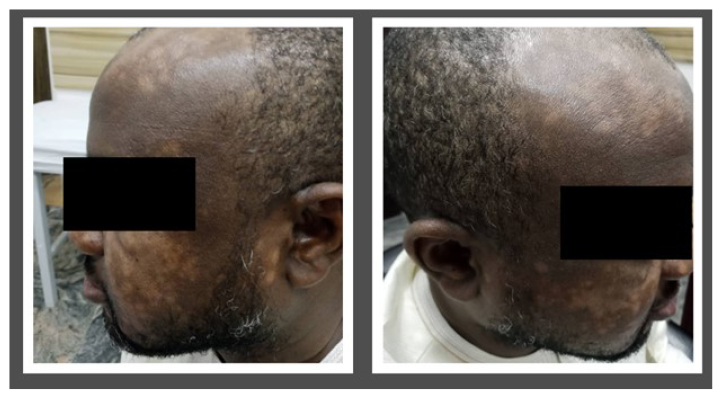
Figure 1: Facial manifestation of vitiligo with multiple hypopigmentations.
Investigation
The diagnosis of vitiligo was first made clinically based on history and physical examination. However, the authors considered seborrhoeic dermatitis as a differential diagnosis as a result of the extensive facial and forehead lesions. On further review of the prior unsuccessful treatments received by the patient, the authors observed that seborrhoeic dermatitis was initially treated unsuccessfully. Another differential is eruptive hypomelanosis, an exanthem suspected to be related to viral infections. However, eruptive hypomelanosis is commonly found in young children aged 2–10 years, with an associated flu-like symptom. The authors’ case was completely different from eruptive hypomelanosis.
Clinically, the extensive depigmentation and hypopigmentation in the face and trunk strongly suggested a diagnosis of vitiligo. Thus, a skin biopsy was completed to establish the diagnosis and for histological diagnosis of vitiligo. The histology report revealed a total absence of functioning melanocytes in the lesions (Figure 2). There was depigmentation juxtaposed with hypopigmentation, suggestive of an ongoing destructive process. Some melanin dissoluteness at the superficial dermis was engulfed by macrophages. There was associated mononuclear, perivascular, and inflammatory cell infiltrate. The epidermal architecture was not significantly altered.
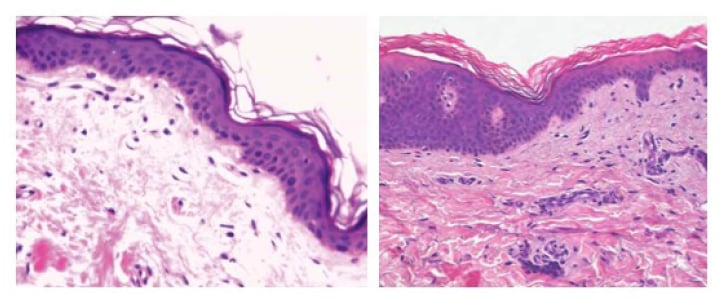
Figure 2: Histopathological features of vitiligo-like hypopigmentation, showing irregular epidermal hyperplasia.
A) Scanty perivascular inflammatory infiltrates were detectable in the superficial dermis. The reduction of melanocytes was confirmed by S100 staining (haematoxylin and eosin: x20).
B) The total absence of melanin in the basal layer of the epidermis and the absence of melanocytes is compatible with vitiligo (haematoxylin and eosin: x400).
To establish the likely cause of the condition, viral serology for Cytomegalovirus IgM and IgG, herpes simplex virus IgG, antinuclear antibodies, and Epstein–Barr virus (EBV) were completed, but only the EBV serology was abnormal (Table 1).
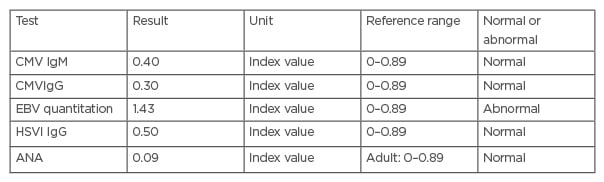
Table 1: Serology test of the patient’s specimen showing Epstein–Barr virus abnormality.
ANA: antinuclear antibodies; CMV: Cytomegalovirus; EBV: Epstein–Barr virus; HSVI: herpes simplex virus I.
The patient was treated with psoralen and ultraviolet A, melatonin, and topical steroids. In addition, to treat the EBV infection, they were placed on valaciclovir, spironolactone, and ivermectin, based on evidence supporting their efficacies.1-3 The patient progressively recovered within 3 months of treatment. Another serology test after 3 months of treatment revealed a reduction of the EBV values from 1.43 to 1.08. However, a complete viral clearance is expected to take a longer time.
DISCUSSION
Vitiligo is an acquired depigmenting disorder that is progressive and has multifactorial aetiopathogenesis. It usually presents with the appearance of circumscribed white macules, papules, and depigmented patches in the skin.4 Empirical evidence shows that vitiligo significantly impacts patients’ emotions and psychology to varying degrees.5 While coping may be easier for those who have the disorder in the non-exposed part of their skin, the psychological trauma may be profound in exposed areas such as their face, as seen in the authors’ patient. For the authors’ patient, the presence of this lesion in their face led to low self-esteem, emotional destabilisation, social anxiety, and avoidance of public places. They also claimed to have spent much money on treatment with no significant changes. Hence, a desire to establish the cause and permanent solution motivated his presentation.
A close differential to the facial presentation of vitiligo is seborrhoeic dermatitis, a chronic inflammatory skin disease impacting the regions of the body rich in sebaceous glands. It is common in the scalp, face, and upper trunk. In adults, seborrhoeic dermatitis results in a chronic remitting and relapsing disease.6 Based on the closeness of this differential, the authors’ patient received initial treatment for seborrhoeic dermatitis in another facility before presenting at their dermatology clinic. However, the treatment for seborrhoeic dermatitis was unsuccessful, as the patient noticed an extensive increase in the lesions. While the authors cannot establish a possibility of the wrong diagnosis by the initial clinical assessor, they considered a diagnosis of vitiligo with a possibility of the Koebner phenomenon as the explanation for the extensive facial manifestation. Mufutau et al.7 earlier noted that the Koebner phenomenon, induced by seborrhoeic dermatitis, may be a perpetrating factor in vitiligo, with an attendant challenge in the treatment of the patients.
Therefore, the authors deemed it necessary to go beyond clinical judgment in diagnosing this case. The histology result confirmed their suspicion, yet the authors explored the possible association of a viral infection with vitiligo. A finding of the EBV in the serology assay prompted a need to report this case as a lesson for clinicians, especially in resource-poor countries. Thus, this report could guide the clinicians on some of the management approaches to vitiligo.
Vitiligo is more common in Africa relative to other parts of the world. Globally, a prevalence rate ranging between 0.2–2% has been reported.9 However, a meta-analysis reported a higher rate in Africa and predominance among females.9 In Nigeria, the prevalence ranged from 0.96 in Northwest Nigeria to 5% in the South.10,11 Another Nigerian study reported the facial presentation of vitiligo as the most prevalent among Nigerians.11
The aetiopathogenesis of vitiligo is multifactorial. Several studies have established a strong correlation between autoimmune disorders and the development of vitiligo.4,8-13 As a result of the established association between viral infections and many autoimmune disorders, recent attention has been drawn to investigating the viral cause of vitiligo. For example, Grimes et al.14 reported Cytomegalovirus positivity in patients with vitiligo.
Primary infection with EBV is mostly asymptomatic until the individual reaches adolescence or adulthood, where it can manifest as infectious mononucleosis.3 EBV is linked to various malignancies, including Burkitt lymphoma, nasopharyngeal carcinoma, Hodgkin lymphoma, and lymphoproliferative disease, irrespective of the individual’s immune status.8 The virus usually becomes latent in memory B cells. The EBV genome replicates when B cells divide using the host DNA polymerase, leading to reactivation. Therefore, valaciclovir has been shown to block the viral replication and decrease the latent EBV load at a rate equivalent to the half-life of memory B cells.3
To the best of the authors’ knowledge, their report would be the first to report a positive EBV serology in a subject from Nigeria, with a histologically confirmed clinical diagnosis of vitiligo. The finding of EBV in this patient suggests a need to pay more attention to the viral association of vitiligo in immunocompetent individuals.
Vitiligo is a recurring depigmenting condition with a possibility of the development of the Koebner phenomenon in up to one-third of the patients.7 Koebner phenomenon, which is the presence of new skin lesions at a distant site, has been reported to worsen treatment and prevent recovery in patients. Infections are identified as one of the causes of Koebner phenomenon.15 Hence, identifying EBV in this patient may explain the possibility of this phenomenon.
Although the authors’ patient was initially treated for seborrhoeic dermatitis with no improvement, an index of suspicion to establish the diagnosis of vitiligo and possible associated risk factors provide an opportunity for proper treatment of the condition. While the authors may not be able to establish a causal relationship between EBV and vitiligo, due to the chronic nature of the disease, they did show an association. Although their patient denied any prior diagnosis of infectious mononucleosis, Burkitt lymphoma, and other related malignancies, establishing the presence of EBV and providing treatment may proactively prevent a future manifestation of any of the EBV-related disorders. However, regular monitoring of the clearance of the EBV viral load in his system for one year is necessary.
A limitation of the authors’ report is that they only reported EBV based on the serology assay. They could not complete PCR testing and viral quantification testing due to the paucity of funds. One major limitation in their practice setting is that the serology testing for these viruses is not readily available, and the cost is not covered by insurance. Hence, patients would need to pay out of pocket. With more reports like this one, the authors anticipate increasing awareness, supporting the advocacy for serological and PCR testing for some viral aetiology of certain autoimmune conditions.






