BACKGROUND
Erosive pustular dermatosis of the scalp (EPDS) is an inflammatory disorder of unknown aetiology, characterised by erosions, pustules, and crusts on a bed of atrophic skin.1-7 Risk factors include elderly age, actinic damage, androgenetic alopecia, and preceding trauma.1-7 It has long been considered a rare disease but recent reports suggest that it may be more frequent than previously thought.
MATERIALS AND METHODS
The authors conducted a retrospective, observational, multicentre study. They reviewed records of patients with clinically and histologically confirmed EPDS for baseline characteristics, time to diagnosis, treatments received, and outcomes. Treatment options included potent topical steroids (TS) under occlusion, topical calcineurin inhibitors (TCi) usually under occlusion, and systemic retinoids. A cycle of TS was defined as daily application for 2 weeks, followed by gradual de-escalation for a further 2 weeks. Follow-up visits were scheduled every 4 weeks. Outcomes were recorded as complete response (complete clinical resolution), partial response (30% or higher reduction of the affected area), progressive disease (20% or higher increase of the affected area), and stable disease. Deterioration and recurrence were defined as at least 20% loss of previous partial response and complete response, respectively. The statistical package STATA version 14.2 (StataCorp, College Station, Texas, USA) was used for data analysis. Twenty-four patients (22 males, two females) were included in the study. The majority were photodamaged (n=20/24 [83.3%]). The most commonly affected site was the vertex (n=19/24 [79.2%]). Twenty-two individuals (91.7%) had a positive non-melanoma skin cancer history, with actinic keratoses (AK) being the most frequently observed type (n=18/24 [75.0%]). Most patients had been treated with cryotherapy (n=17/24 [70.8%]) and imiquimod (n=14/24 [58.3%]).
RESULTS AND DISCUSSION
At first follow-up visit, from 22 patients treated with TS, 14 (63.6%) showed complete response, seven (31.8%) partial response, and one (4.6%) stable disease. After treatment cessation, the majority (78.3%) experienced a recurrence or deterioration at a median time of 8 weeks (interquartile range: 4–12 weeks; range: 2–16 weeks). Recurrence or deterioration was managed with either a TS cycle combined with 25 mg of acitretin daily (acitretin was continued after TS withdrawal as maintenance treatment); a TS cycle followed by TCi as maintenance treatment; or TCi in combination with 25 mg of acitretin, both in continuous application. New recurrences were observed in two out of nine patients (22.2%) that received acitretin, and in five out of seven patients (71.4%) that received TCi as maintenance (Figure 1)
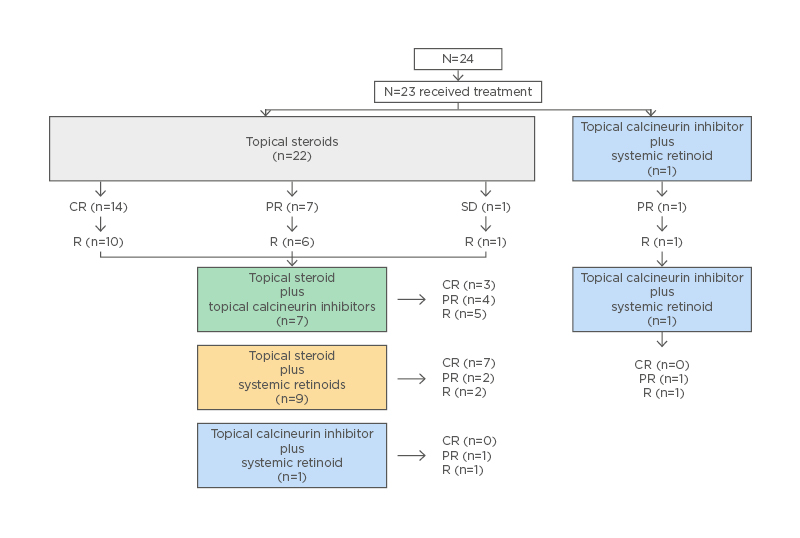
Figure 1: Erosive pustular dermatosis of the scalp treatment flowchart. CR: complete response; PR: partial response; R: recurrence/deterioration; SD: stable disease.
The authors’ descriptive analysis of baseline characteristics of patients with EPDS conform with most recent publications.4,6,7,8 EPDS is diagnostically challenging due to a clinical overlap with other entities, including non-melanoma skin cancer, fungal/bacterial infections, bullous dermatoses, and folliculitis decalvans.4,5,9,10 Considering that it often develops in the background of field cancerisation, presence of actinic damage in the skin specimen may act as a misleading feature for the pathologist too, who may ultimately report the lesion as actinically damaged skin. The latter may result in further topical/destructive therapies that maintain the vicious circle of inflammation-impaired healing.
The management of EPDS is also challenging. Despite its responsiveness to TS,3,4,6,10 recurrence after treatment cessation is the rule.3,4,6,10 Prolonged use of TS cannot be considered since the latter promotes skin atrophy, which plays a key role in EPDS pathogenesis. Epidermis-preserving strategies, such as systemic retinoids or TCi, are desirable.
CONCLUSION
According to the authors’ results, systemic retinoids appear to be a superior form of maintenance treatment compared with TCi. Study limitations derive from its design, and the small sample size may create confounding and bias.







