BACKGROUND
Hidradenitis suppurativa (HS) is a chronic, incurable disease of apocrine gland-bearing skin, which presents with painful nodules and scarring most commonly in the axillae, inguinal, and inframammary folds. Comorbidities associated with HS often include increased rates of depression and anxiety, and patients tend to come from lower socioeconomic backgrounds with higher rates of unemployment.1,2 There is a paucity of highly effective therapies available for HS patients, with no proven therapeutic basis for complementary and alternative medicine (CAM).3 This study investigated CAM use in a cohort of patients with HS attending a monthly tertiary specialist HS clinic over a 4-month period (N=139; 107 completed questionnaires).
Patients were asked to respond to nine questions on previous CAM use, concerning rationale, duration, cost, treatment success, duration of HS, and previous HS-related hospital admissions.
RESULTS
Results showed that 20.0% of patients had previously used a CAM, with an extensive range of treatments reported including turmeric, reiki, acupuncture, and aromatherapy (Table 1). A number of reasons were reported for CAM use in the patient population, the most common being curiosity and dissatisfaction with conventional treatment (Table 1). One patient believed CAM had no potential to cause adverse effects while another patient was employed as a complementary therapist themselves. Eight patients reported a decrease in symptoms and an increase in quality of life with CAM use (38.1%). Patients had spent between €0.00 and €5,200.00 on CAM treatment, with an average cost of €413.55, and therapy duration range from 1 week to 2 years. Acupuncture (€50.00/session), reiki (€30.00/session), and aromatherapy (€25.00/session) were the most expensive treatments, while turmeric was the cheapest costing a maximum of €5.00. The mean duration of HS was 13.1 years and almost 50% of patients had been admitted to hospital for HS treatment (n=40). Only three patients had been questioned previously by a doctor regarding CAM use.
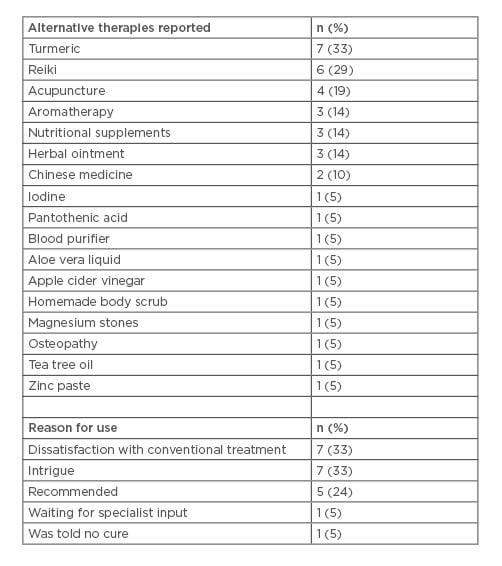
Table 1: Alternative therapies reported and reasons for use.
CONCLUSION
In the cohort of patients with HS, use of CAM was lower than reported in the general population.4 This under-representation in the patient population was potentially due to the accessibility of conventional treatments at this specialist HS clinic. The practice of alternative medicine is increasingly endorsed by celebrities and influencers on social media platforms, with turmeric labelled a ‘wonder drug’ in the media.5 There is, to date, little legislation regarding use of social media to promote treatments without proven therapeutic effect as ‘instagrammers’ with millions of followers promote controversial products.6 As HS is a disease characterised by lower socioeconomic status and increased comorbidity burden, the use of expensive, ineffective, and dangerous treatments should be discouraged. Patients most commonly reported CAM use due to curiosity and one patient believed alternative medicine had no side effects when compared to conventional HS treatments. Most dermatologists do not enquire about alternative therapies but given that negative outcomes and serious adverse events are widely reported in the literature,7 routine questioning for all patients with HS should be encouraged.
Dermatologists should familiarise themselves with alternative treatments so that open and honest dialogue can enable patients to make an informed decision regarding their ongoing CAM use in the age of Instagram, social media influencers, and sponsored celebrity endorsements.







