INTRODUCTION
Metformin, a widely used antidiabetic and antiobesity drug, exerts multiple effects on the skin, and could potentially induce a variety of dermatoses.1 Among others, the most commonly described drug-induced skin reactions include rash, urticaria, and lichenoid eruption.2,3
CASE REPORT
The authors herein report a rare case of generalised erythema annulare in a 75-year-old female Caucasian patient with multiple comorbidities. The skin eruption was presented by polycyclic out-spreading erythematous lesions, with central clearing. Concomitant pathology included Type 2 diabetes mellitus, hypertension, coronary heart disease, coronary stent implantation, atrial fibrillation, mitral regurgitation, chronic obstructive pulmonary disease, chronic respiratory failure, Hashimoto’s thyroiditis, hip arthroplasty, chronic gastritis, caecal and ascending colon polyps, and secondary iron deficiency anaemia. The concomitant therapy included metildigoxin, bisoprolol, valsartan, furosemide, acenocoumarol, spironolactone, pantoprazole, rosuvastatin, levothyroxine, metformin, allopurinol, fluticasone furoate/vilanterol, and tiotropium.
Histopathological examination of a skin biopsy showed a thinned epidermal layer and a tight lymphocytic infiltrate in the upper dermis containing eosinophils and surrounding the vessels in a ‘coat-sleeve’ distribution. Based on the characteristic clinical and histological appearance of the skin lesions, a diagnosis of erythema annulare centrifugum (EAC) was given. Therapy with topical clobetasol propionate 0.05% cream was started, as well as consecutive replacement of the concomitant medications. Only the exclusion of metformin led to the disappearance of the skin lesions in 2 weeks. No relapse of the EAC occurred thereafter.
DISCUSSION
First described by Darier in 1916,4 EAC is a reactive condition that can be associated with drug intake. A list of the known drug-induced skin reactions to metformin are presented in Table 1.5-28 The exact mechanisms on the development of skin reactions include Type IV hypersensitivity, circulating immune complex deposits, immunological or/and nonimmunological release of proinflammatory factors, components of the complement, derivatives of the prostaglandin pathways, cytokines, and cytotoxicity.5-13
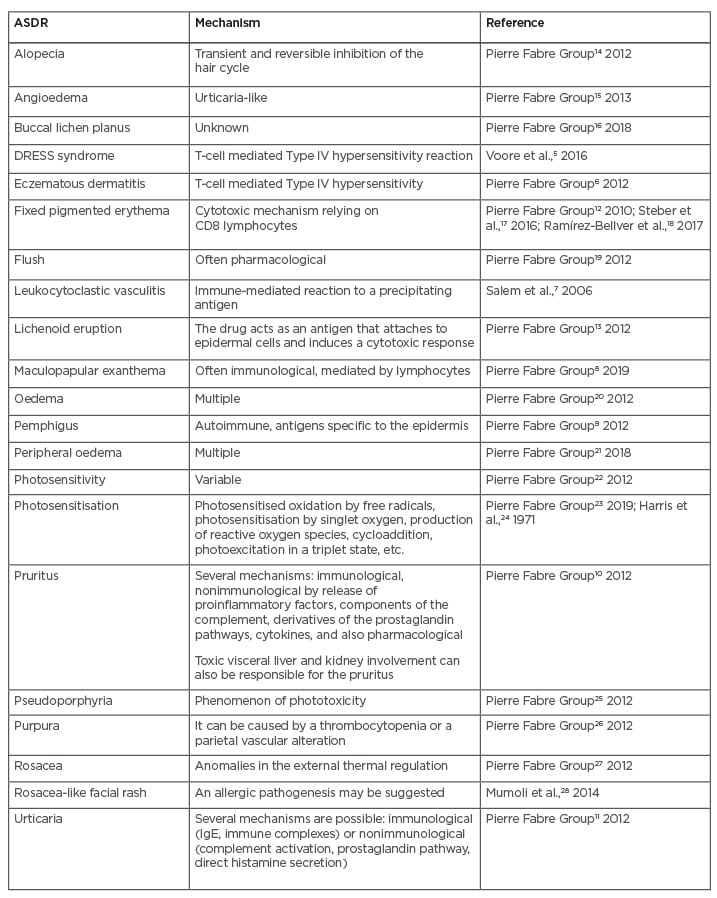
Table 1: A list of the known drug-induced skin reactions to metformin.
CD: cluster of differentiation; DRESS: Drug rash with eosinophilia and systemic symptoms.
CONCLUSION
The pathophysiology of drug-induced EAC probably includes a variety of mechanisms, and thus leads to versatile clinical manifestation. In this case of generalised EAC, only via the exclusion of metformin from the patient’s therapy did their skin lesions resolve. Therefore, it seems most likely to have been responsible for the disease development.







