BACKGROUND AND AIMS
COVID-19 primarily affects the respiratory system of patients; however, the cardiovascular system is also damaged. To study the impact of a novel coronavirus infection on the cardiovascular system, in particular on echocardiographic parameters after severe acute respiratory syndrome coronavirus-2, is therefore very important.
The aim of this study was to compare echocardiographic parameters in patients with COVID-19 pneumonia in hospital and 3 months after hospital discharge.
MATERIALS AND METHODS
The patients were identified according to the data of the medical information system of the monohospital from April to July 2020, within the framework of the ‘One-year Cardiac Follow-up of Patients With COVID-19 Pneumonia’ trial,1 3 months±2 weeks after discharge. The inclusion criteria were a documented diagnosis of COVID-19-associated pneumonia, age ≥18 years, and the patient’s desire to participate in follow-up. The authors did not include patients with chronic diseases in the acute stage, heart defects, HIV, chronic hepatitis, cancer under 5 years, tuberculosis, and other diseases accompanied by pulmonary fibrosis. The exclusion criteria were a refusal to participate, pregnancy, and unsatisfactory visualisation by echocardiography. Eight patients were excluded: two due to departure in another region, three due to pregnancy, and three due to refusal to undergo dynamic CT lung screening. A total of 106 men and women were included. Mean age was 47 years (standard deviation: ±16 years; range: 19–84 years), mean BMI was 28.2 kg/m2 (standard deviation: ±5.7 kg/m2), and 49% were female. During hospitalisation, chest CT detected mild lesions in 29.2%, moderate lesions in 31.1%, severe lesions in 27.4%, and critical lesions in 5.7% of patients.
RESULTS
Cardiovascular diseases were detected in 52% of patients. Three months after discharge, complaints persisted in the majority of patients (86%). Three months after discharge, significant decreases in left ventricular (LV) end-diastolic, end-systolic, and stroke volumes were noted (Table 1). A tendency to decrease the systolic volume of the left atrium was found. There were no dynamics from the linear left atrium parameters and LV ejection fraction. The frequency of significant tricuspid regurgitation in hospital was 2.4%, and it did not change within 3 months. End-diastolic right ventricular outflow tract diameter and pulmonary artery trunk diameter became significantly lower, as well as average systolic pulmonary artery pressure. As for the right atrium, its average volume and width decreased, and its length increased. Three months after discharge, the rate of right ventricular dilatation in the authors’ patients was 2.9% and the rate of tricuspid annular plane systolic excursion decrease was 9.5%.
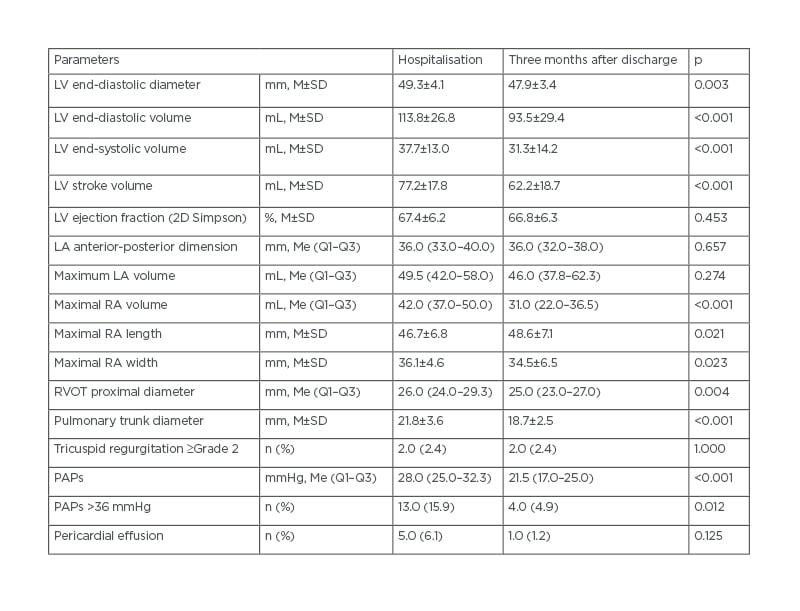
Table 1: Dynamics of echocardiographic parameters in patients survived COVID-19 pneumonia (n=106).
LA: left atrium; LV: left ventricular; M: mean; Me: median; n: portion of patients; PAPs: systolic pulmonary artery pressure; Q1: quartile 1; Q3: quartile 3; RA: right atrium; RVOT: right ventricular outflow tract (parasternal view, long axis); SD: standard deviation.
DISCUSSION
To date, three European research groups have published the results of observation 3 months after hospitalisation with COVID-19.2-4 Echocardiographic data was studied only by the Austrian group.4 According to the observation of 145 Austrian patients, the LV ejection fraction was reduced in four out of 133.4 In the authors’ work, it was reduced in two out of 106. The frequency of pulmonary hypertension and a decrease in LV ejection fraction in the Austrian cohort did not change over 3 months after discharge. Additionally, the number of patients with pericardial effusion decreased.4 In the present study, the number of patients with echo signs of pulmonary hypertension significantly decreased. Furthermore, the number of patients with pericardial effusion also decreased; however, these differences did not reach significance.
CONCLUSIONS
In patients after COVID-19 pneumonia, echocardiography showed decrease of the load, predominantly on the right heart 3 months after discharge. In 86.0% of patients, complaints persisted. Cardiovascular diseases were detected in 52.0% of the patients, including arterial hypertension in 48.1% and coronary artery disease in 15.1%.








