BACKGROUND AND AIMS
TGF-β1 is a crucial regulatory cytokine that contributes to the development of the mitral valve. Under normal conditions, TGF-β regulates extracellular matrix protein synthesis in valvular interstitial cells.1 Growing evidence supports the role of TGF-β as a mediator of the myxomatous changes in syndromic and non-syndromic mitral valve prolapse (MVP).2,3 Upon changes in the TGF-β expression, valvular interstitial cells acquire features of activated myofibroblasts, proliferate, and produce increased amounts of collagens, proteoglycans, and metalloproteases, which are responsible for the remodelling of collagen and elastic fibres in mitral leaflets.4 To evaluate the effect of elevated circulating TGF-β level on the progression of the valve myxomatosis and leaflets billowing at long-term follow-up, the authors conducted an observational, prospective, single-centre study.
MATERIALS AND METHODS
Seventy-eight asymptomatic young subjects (mean age: 19.7±1.6 years; 72% male) with MVP were consecutively enrolled in the authors’ observational, prospective, single-centre study. MVP was diagnosed by billowing one or both mitral leaflets >2 mm above the mitral annulus in the long-axis parasternal view. Concentration of TGF-β1 in serum was determined by ELISA using test system Human Platinum ELISA (Thermo Fisher Scientific, Waltham, Massachusetts, USA).
RESULTS
During 1,170 person-years of follow-up (median: 14.5 years), no deaths or MVP-related events occurred. Posterior leaflet’s thickening (from 3.9±1.4–4.4±1.7 mm [diameter (D): +0.5 mm]; p<0.01) and increase of the billowing (progression in maximal prolapse depth from 3.5±2.4–4.8±2.8 mm [D: +1.3 mm]; p<0.001) leads to the mitral regurgitation progression (vena contracta: 2.3±0.4 mm versus 3.5±0.4 mm [D: +1.2 mm]; p<0.0001) over 15 years of follow-up.
TGF-β1 serum level was increased (15.2±12.3 ng/mL) and strongly correlated with the thickening of the posterior leaflet (effective size estimate: 0.72; p=<0.0001 [ Figure 1 ]). In multivariate Cox analysis, the TGF-β1 level was the independent predictor of the posterior leaflet’s thickening (2.07; 95% confidence interval [CI]: 1.34–3.29; p=0.001) and progression of the billowing (2.89; 95% CI: 1.61–4.37; p=0.0001).
TGF-β1 >7.0 ng/mL was a strong predictor (area under the receiver operating characteristic curve: 0.84; 95% CI: 0.7–0.9; sensitivity: 82%; specificity: 95% [ Figure 1 ]) for progression of MVP (maximal prolapse depth increase: D+1.9±1.2 mm [TGF-β1: >7.0 ng/mL] versus 0.7±0.6 mm [TGF-β1: <7.0 ng/mL]; p<0.0001) and mitral regurgitation (vena contracta increase: D+1.5±0.5 mm [TGF-β1: >7.0 ng/mL] versus 0.5±0.4 mm [TGF-β1: <7.0 ng/mL]; p<0.0001).
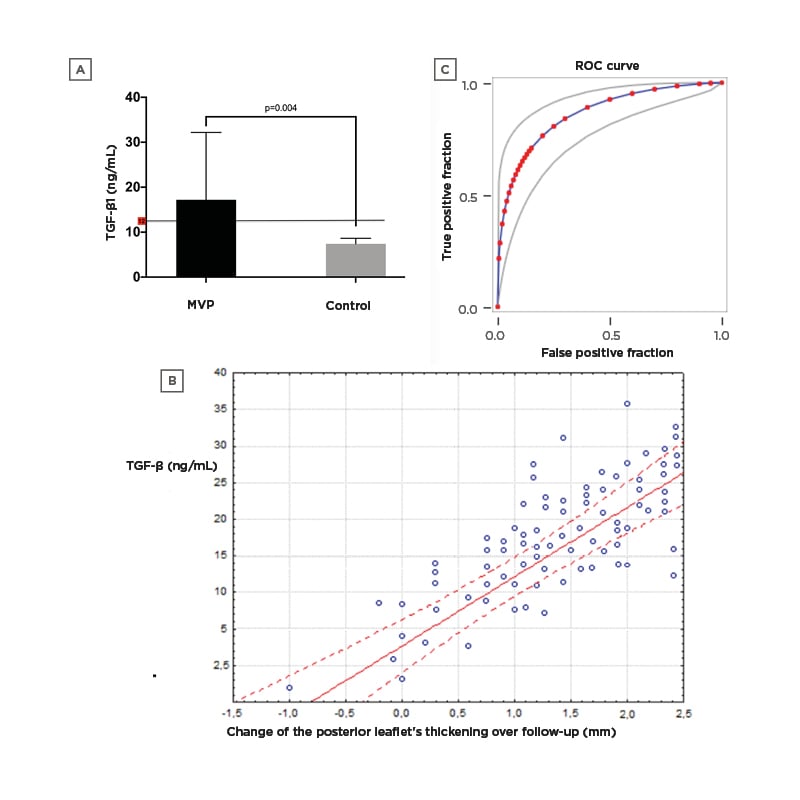
Figure 1: Increasing plasma TGF-β1 in patients with MVP.
Plasma TGF-β1 level increased in patients with MVP when compared to controls (A). Regressions showing the correlation between plasma TGF-β1 concentrations and the thickening of the posterior leaflet during the follow-up (B). Graphical representation of the ROC analysis (C). MVP: mitral valve prolapse; ROC: receiver operating characteristic.
CONCLUSION
Despite the overall benign prognosis, the authors found the obvious echocardiographic progression of the valve myxomatosis and leaflets billowing in a long-term follow-up in young people. Elevated above 7.0 ng/mL, TGF-β1 serum level might serve as a prognostic biomarker and identify patients with increased risk of the MVP progression.








