Authors: Christopher Chapple1,2,3,4 Arnulf Stenzl5,6
1. Consultant Urological Surgeon, Sheffield Teaching Hospitals NHS Foundation Trust
2. University of Sheffield
3. Sheffield Hallam University
4. Secretary General, European Association of Urology (EAU)
5. Secretary General Adjunct, European Association of Urology (EAU)
6. Chairman of Urology, University of Tübingen Medical Center, Germany
*Correspondence to [email protected]
Citation: EMJ Urol. 2021;9[1]:25-29.
INTRODUCTION
The European Association of Urology (EAU) held its 36th Annual Congress, EAU21, on 8th–12th July. The global pandemic required the organisers to hold EAU21 virtually, with a small number of session chairs and moderators travelling to the Netherlands to host sessions in a studio setting (Figure 1).

Figure 1: The European Association of Urology (EAU) 2021 studio set in Hilversum, the Netherlands.
Some moderators and sessions chairs were able to travel to ‘host’ the congress and lead discussions.
The congress attracted over 6,200 unique participants from 120 countries. During the congress days, 52,000 live views were logged for the 180 sessions. The five-day EAU21 Scientific Programme featured 1,600 faculty members and speakers discussing all of the latest developments in urology. The European School of Urology (ESU) hosted special courses during congress hours, and a special programme for urology patients was also introduced this year. The European Association of Urology Nurses (EAUN) will hold its own virtual meeting in September.
What follows is an extremely condensed overview of some of the highlights of the EAU21.1
FULL DAY OF SEMI-LIVE SURGERY
‘Technology development never ends!’ was the catch-all title for the nearly eight-hour flagship, semi-live surgical session at the EAU21. The session, or more accurately, the Meeting of the EAU Section of Uro-Technology (ESUT), Robotic Urology Section (ERUS), and Section of Urolithiasis (EULIS) was designed to take up most of the first day of the EAU21, lasting from 10 a.m. to 7 p.m., with an hour-long break at noon. Ali Serdar Gözen and Jochen Walz chaired the day’s sessions.
The first five blocks of presentations covered a wide range of innovations in urological technology, including flexible ureteroscopy with thulium fibre laser, several new kinds of laser technology (including a demonstration of mini-PCNL with MOSES 2.0), and the demonstration of a new kind of ureteral stent, the JFil, by Andrea Bosio. The JFil led to a lot of questions from the audience, who were clearly interested in the potential of the innovative ‘pigtail’ stent and its potential for reducing stent-related symptoms.
A real scoop in this first series of talks was the participation of Ruben Olivares, who was the first to use the Medtronic Hugo RAS system to perform a prostatectomy on June 19th at the Clinica Santa Maria in Chile. Olivares highlighted the system’s modular nature, its flexible upgradeability, the advantages of its open console, and the support for standard surgical tools.
This historic first procedure would mark the start of a registry and data collection on the performance of the system.
NIGHTMARE SESSION
The first Plenary Session of the EAU21 was the Nightmare Session on Friday morning, which was about early detection of prostate cancer. Roderick van den Bergh, Isabel Heidegger, and Armando Stabile each gave a case presentation, which were discussed and then cross-examined by medical lawyer Bertie Leigh afterwards. Besides Leigh, the session was chaired by Chris Bangma and Walz.
van den Bergh described his case as a situation that “started as a fairy tale and ended as a nightmare.” He alluded to it as a perfect case of active surveillance that ended in a “possible metastatic lesion.” Leigh said: “There is nothing wrong with active surveillance. It is a great advance in modern urology. It is about the way you do it and that is what went wrong in this case.”
Later in the session, the focus shifted to low-grade cancers: “The frequent problem of over-treatment,” as Walz put it. The over-treatment case presented was quite unique as the patient had put pressure on his urologist to perform a radical prostatectomy, which raised the question: what if a patient keeps pushing for surgery? Leigh stated: “When your patient asks you to do something that you think will do him harm and will not do him any good, you should rarely comply with his wishes.”
MANAGEMENT OF INCONTINENCE
Centred on the optimal management of incontinence in elderly patients, Plenary Session 2, which took place on Friday, also covered what drug interactions to be aware of when using pharmacotherapy for urgency urinary incontinence. According to Martin Michel, complete medication history is key to the prevention, detection, and management of drug–drug interactions.
EAU Secretary General, Chris Chapple, discussed that new mesh materials need to be more like a fascia-mimetic material, which is made of three layers of polyurethane electro-spun fibres. Polyurethane materials cope well with repeated distension and are well-tolerated in animals, inducing little inflammation.
Mary Lynne van Poelgeest-Pomfret underscored the importance of listening to patients with regard to treatment goals and evaluation tools.
ADVANCED BLADDER CANCER IN 2021
Plenary Session 3, ‘Advanced bladder cancer in 2021: Going forward?’ on Saturday morning, looked into the future of advanced bladder cancer treatment. Chaired by Maria De Santis, Joan Palou, Morgan Rouprêt, and Arnulf Stenzl, the session went into technical advances and personalised and targeted therapeutic strategies.
James Catto kicked-off the session with his state-of-the-art lecture ‘Safe and optimal management of muscle-invasive bladder cancer (MIBC) in the time of SARS-CoV-2.’ He said: “In terms of cure [for MIBC], we have two choices: surgery or radiotherapy.” He went on to present the pros and cons of each of these approaches in light of COVID-19 (Figure 2).
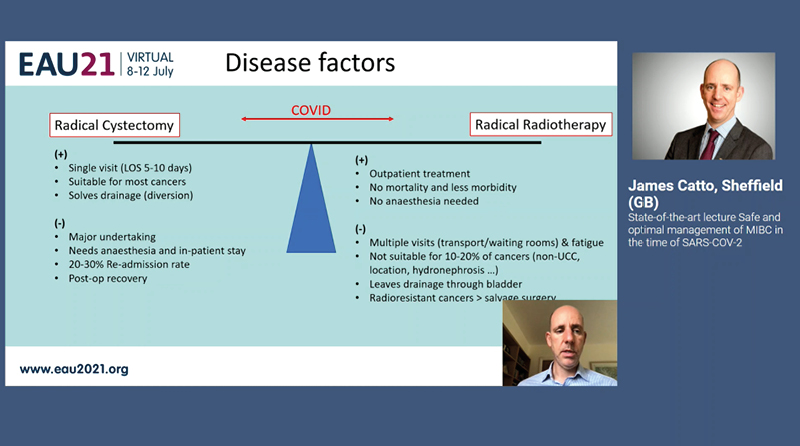
Figure 2: The pros and cons of radical cystectomy versus radical radiotherapy in light of COVID-19.
LOS: late-onset sepsis; UCC: urothelial cell carcinoma.
The second state-of-the-art lecture was given by Lars Dyrskjøt, who answered the question of whether it is possible to use molecular markers to decide treatment for MIBC. One of his conclusions was that “ctDNA [circulating tumour DNA] has many opportunities across the patient disease course to inform clinical practice.”
The final state-of-the-art lecture of the session was Enrique Grande’s ’Does every metastatic patient need immunotherapy in a first-line setting?’ pertaining to metastatic urothelial carcinoma. Grande started his lecture by answering his central question with a “probably not;” he ended with a “definitely not.”
RENAL CANCER
Plenary Session 4 addressed updates on localised and metastatic renal cancer. W. Marston Linehan kick-started the session with his Society of Urologic Oncology (SUO) lecture on the discovery, oxygen sensing, and therapy using the von Hippel-Lindau (VHL) kidney cancer gene.
To find the gene for clear cell renal cell carcinoma, Linehan and his team conducted genetic linkage in families affected with VHL disease. They localised the gene to the short arm of chromosome 3 and, with physical mapping, identified the VHL gene, which is a two-hit, loss-of-function, tumour-suppressor gene. Linehan also cited the relevance of the findings of the Nobel Prize-winning study on how cells can sense and adapt to changing oxygen availability.
Covering immunotherapy-based management of metastatic clear cell and variant renal cell carcinoma, Ignacio Duran stated that immunotherapy-based combinations can provide a long-term benefit in a substantial percentage of patients with metastatic clear cell renal cell carcinoma.
Moderated live from the EAU21 studio, Umberto Capitanio, Marc-Oliver Grimm, and Peter Mulders chaired Plenary Session 4.
METASTATIC PROSTATE CANCER
On Sunday, Plenary Session 5 commenced and focused on the treatment for metastatic hormone-sensitive prostate cancer. The session was led by Alberto Briganti, Karim Fizazi, Silke Gillessen Sommer, and Arnauld Villers.
During his state-of-the-art lecture, Declan Murphy emphasised that in the de novo setting, the accuracy of prostate-specific membrane antigen PET/CT is superior to conventional imaging.
Later in the session, Christopher Sweeney said that there is evidence to support the hypothesis that men with metastatic hormone-sensitive prostate cancer have a wide array of prognoses, which can be easily defined by clinical variables. In discussions on the role of imaging-guided treatments such as radiotherapy, Pierre Blanchard stated there is a low level of evidence for metastases-directed therapy in the oligometastatic recurrent prostate cancer setting, although metastases-directed therapy is widely used.
EVER-INCREASING APPLICATIONS FOR ROBOTIC SURGERY IN UROLOGY
Robotic urology is a rapidly evolving field, with many studies underway and results coming in the next few years, but some careful conclusions were already drawn by the speakers at the EAU21 on Sunday. Plenary Session 6, chaired by Alex Mottrie, Maarten Albersen, and Timothy O’Brien, examined if the surgical robot is starting to take over reconstructive surgery, traditionally the field for open or laparoscopic techniques, and all signs are pointing to a shift to robotic-assisted surgery.
As departing Chairman of the EAU Robotic Urology Section (ERUS), Mottrie is, understandably, extremely enthusiastic about the potential of robotic surgery and advanced surgical technology in general: “This session proves that everything is becoming robotised. We started with prostate, prostatectomy, then kidney, and bladder, but now everything that we do with our bare hands is going more and more towards robotics. There are new robotic systems coming to market: microsurgery, and so on. This will very probably soon include urethral reconstruction and whatever else. As the expenses come down, also due to increased competition, there are very few drawbacks left.”
While robotic training is becoming increasingly standardised thanks to ERUS, its curriculum, and the work of training centres like Orsi, how much of the current robotic training is based on a single robotic system, and how useful will it be as the market becomes more diverse?
Mottrie stated: “As it currently stands, we only have one system. Our current training protocols are, let’s say, a ‘mono-robot training’. But we will, in the coming years, come to a new era where we will have robot-agnostic training. When you buy a car, sure, there are differences between brands, but the driver’s licence is the same. You might need the company to tell you what each button and switch does, but in terms of surgical technique and approach, it’s all basically the same. It’s work in progress on our part.”
THE PROSPECTS OF SURGICAL REMOTE LEARNING
The final of seven Plenary sessions at the EAU21 took place on Day 5 of the virtual congress, bringing together stone experts from across the continent for an interesting live session. The session was chaired from the studio by Thomas Knoll and Selçuk Silay, joined by Evangelos Liatsikos remotely.
Amid case discussions that weighed the benefits and drawbacks of extracorporeal shock wave lithotripsy, percutaneous nephrolithotomy, or flexible ureteroscopy, was an update on technique and training. Olivier Traxer summarised his personal experiences of remote training over the past fifteen months.
“With the events of 2020, we have had to rethink education,” said Traxer. “Social media has allowed us to get in touch and spread information, but of course there is little in the way of quality control. The industry has started developing webinars and educational platforms, but we must of course admit that there is a certain amount of bias there.
“International societies like the EAU and the European School of Urology (ESU) perhaps did the most to replace physical meetings, creating evidence-based webinars and learning tracks. This year’s Annual Congress [EAU21] is an excellent example of what we are now able to do, to teach surgical theory. Things like stone composition recognition can easily be done from home.
“The fact remains, however, that we are surgeons and we have so far not been able to replace in-person, hands-on teaching. We need feeling and feedback from our tools. While this is so far irreplaceable, a mix of hands-on and remote training is certainly a future for us.”
Knoll and Liatsikos joined in discussing these realities with Traxer. Perhaps remote ‘coaching’ of more experienced surgeons with a live feed of the procedure (similar to moderation during live surgery sessions) is an option, but only if the surgeon already has a degree of skill. There are also many legal ramifications that need to be examined for this to be considered.
Although the congress might have ended, registration remains open for people who would like to watch all the content on-demand. The EAU21 scientific content remains accredited until 12th October 2021, earning participants up to 40 hours of continuing medical education credits.1








