Abstract
Background: Tubular ectasia of the rete testis (TERT) is a dilatation of the seminiferous tubules of the mediastinum testis. It tends to be asymptomatic and usually constitutes an incidental finding of imaging studies. Scrotal ultrasound (SU) shows tubules with a cystic appearance, suggesting a number of possible diagnoses, including testicular tumours.
Objective: To review our experience and describe the clinical and ultrasound features.
Design: Retrospective descriptive review.
Setting: The images were obtained by SU on an ambulatory basis. SU was performed with the Pro Focus Ultrasound System (BK Medical®, Massachusetts, USA). The indications of the exploration, the SU findings, and the associated conditions were the variables analysed.
Participants: 460 SU studies performed in our hospital between 2010 and 2013. The subjects were men, with a median age of 66 years (range 47–78).
Outcome Measurements and Statistical Analysis: SPSS® version 20 (IBM, New York, USA) was used for the descriptive analysis of the data.
Results and Limitations: TERT was identified in 23 out of 460 SU studies performed. SU was indicated due to the presence of scrotal swelling in 7 patients (30%), an epididymal mass in 8 patients (35%), mild testicular pain in 6 patients (26%), and post-surgical control in 2 asymptomatic patients. Within the 23 patients, 10 (43.4%) were diagnosed with an epididymal cyst, 3 (13%) with chronic epididymitis, and 9 (39%) with a hydrocoele. With regard to associated conditions, 3 (13%) had undergone ipsilateral inguinal hernia repair, 3 (13%) had undergone ipsilateral hydrocoelectomy, and 1 (4%) had a history of contralateral testicular cancer. TERT was unilateral in all cases. No malignant degeneration of the lesions was observed in our series.
Conclusions: According to our experience, TERT is an incidental condition where detailed clinical history, adequate physical examination, and SU findings can lead to the diagnosis. Knowledge of this disease is therefore essential for urologists.
Patient summary: In this report we analyse the clinical features and the SU findings associated with TERT, a condition incidentally found in imaging studies of men in their 60s usually performed for other reasons.
INTRODUCTION
Tubular ectasia of the rete testis (TERT) is a dilatation of the seminiferous tubules of the mediastinum testis. At ultrasound the tubules present with a cystic appearance.1-3 Intratesticular cystic lesions include simple cysts, epidermoid cysts, TERT, intratesticular varicocoele, and abscesses. The true relevance of intratesticular lesions lies in their differential diagnosis (including testicular cancer), principally in young adults where they are most commonly diagnosed. An adequate diagnosis is therefore very important to avoid unnecessary imaging studies such as magnetic resonance imaging (MRI) or orchidectomy.1 An ultrasound diagnosis is not difficult to establish but a series of guidelines, which are commented upon in this study, must be taken into account.3,4
Most publications include a single case report or a series; for example, Burrus et al.,1 which included 13 patients or Ortega et al.,5 which included 19 patients. As far as we know, our series is one of the largest in the published literature. The objective is to review our experience in TERT diagnosis and management, and describe both clinical and ultrasound features.
METHODS
We conducted a retrospective study and reviewed 460 scrotal ultrasound (SU) studies performed in our hospital between January 2010 and November 2013. The images were obtained by SU in an outpatient setting; the patients were males attending the ultrasonography room. The indications for exploration ranged from testicular pain to swelling or suspected epididymal mass.
The variables analysed were age, presence of scrotal mass, swelling, pain, and trauma. SU findings categorised as ‘normal images’ included epididymal cysts, chronic epididymitis, hydrocoeles, testicular ischaemia, and haematocoeles. The associated conditions evaluated were cryptorchidism and inguinal hernia, and a history of orchidopexy, vasectomy, epididymectomy, previous hernia repair, hydrocoelectomy, as well as other medical conditions such as cirrhosis or end stage renal disease (ESRD) on haemodialysis or peritoneal dialysis.
SU studies were carried out using the Pro Focus Ultrasound System (BK Medical®, Massachusetts, USA) equipped with a small-part probe operating at a frequency of 8.0–12.0 MHz. Patients were received in the ultrasound exploration room and required no prior preparation of any kind. Exploration was performed in the supine decubitus position, with an estimated duration of 10–15 minutes. The lesions were located by obtaining a sagittal view of the testicle, with the mediastinum testis at the centre. TERT was diagnosed when cystic images were detected, mostly with a tubular or rosary-like morphology of variable number (usually >10) grouped at the upper pole of the testicle. Clear circumscribed circular images appeared to constitute independent cysts, though in most cases modification of the direction of the ultrasound beam showed that these elements correspond to normal tubules acquired in cross-section. Colour Doppler sonography revealed the absence of internal flow inside the cystic lesions, differentiating them from intratesticular varicocoele (Figure 1).
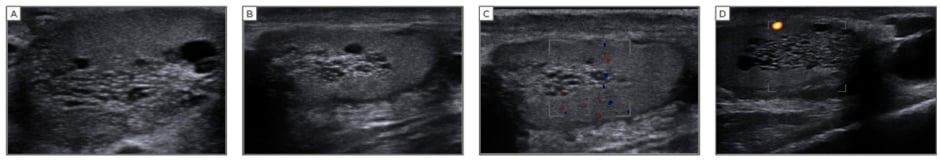
Figure 1: Ultrasound with and without added Doppler imaging showing tubular structures in the mediastinum testis lacking vascular flow.
RESULTS
Among the 460 ultrasound studies performed, TERT was identified in 23 patients (5%) aged between 47 and 78 years (median 66 years) in the stated time period. TERT was found to affect up to two-thirds of the longitudinal diameter of the testicle in some cases. The mean size of the anechoic images was 0.7 mm.
In our series, ultrasound exploration was indicated due to scrotal swelling in 7 of the 23 patients (30%), epididymal masses in 8 cases (35%), mild testicular pain in 6 patients (26%), and post- surgical control in 2 asymptomatic patients (9%) (Figure 2). No indications were given after testicular trauma. Regardless of the indication, 10 of the 23 patients (43%) were diagnosed with epididymal cysts and 3 (13%) were diagnosed with chronic epididymitis, while 9 (39%) presented with a hydrocoele, and 1 (4%) had non-associated findings (Figure 3).
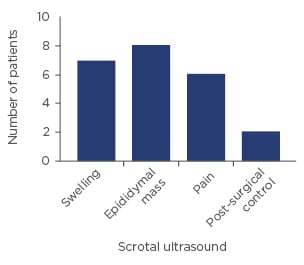
Figure 2: Scrotal ultrasound indication.
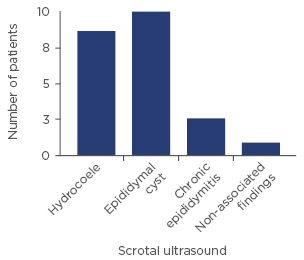
Figure 3: Scrotal ultrasound findings.
A number of associated conditions were observed; 3 patients (13%) had undergone ipsilateral inguinal hernia repair and 3 (13%) had undergone ipsilateral hydrocoelectomy, while 1 patient (4%) had a history of contralateral testicular cancer. This patient, a 54-year-old male, had been diagnosed with a Stage 1 testicular seminoma 20 years previous to the study.
None of the other factors that have previously been associated with this condition in the current literature, such as orchidopexy, vasectomy, epididymectomy, and other medical conditions such as cryptorchidism, cirrhosis, or ESRD with haemodialysis or peritoneal dialysis as a treatment were observed in this series of patients. Furthermore, none of our patients presented bilateral lesions.
DISCUSSION
The rete testis is formed by the confluence of the seminiferous tubules which fold to form a compact structure within the mediastinum testis and merge in the efferent ducts, which conform the epididymal head.5 From an aetiological perspective, obliteration of the seminiferous tubules, due to either luminal obstruction or external compression, causes the formation of the cystic dilatations that characterise this condition. The tubules may contain spermatozoa and can be connected to the lumen of non-dilated ducts in cases of partial obstruction.
According to the existing literature, TERT is a condition that affects middle-aged men and its prevalence increases with age;6 in our series, the youngest patient was 47 years old. Nevertheless, most diagnoses correspond to patients in the sixth decade of their life and onwards. From a clinical point of view, TERT tends to be asymptomatic at the time of diagnosis and often constitutes an incidental finding in imaging studies performed for other indications.
To date, a number of factors have been related to the disease, including epididymal alterations such as cysts, chronic epididymitis, or epididymectomy, as well as space-occupying lesions such as testicular tumours. Haematocoele has been described as a cause of extrinsic tubular compression. Other causes are cryptorchidism and vasectomy. From a systemic point of view, cirrhosis has been described as a possible triggering factor, giving rise to hormonal alterations that can lead to ischaemia of organs such as the testes. Other systemic causal factors are haemodialysis or peritoneal dialysis secondary to the accumulation of calcium oxalate crystals within the tubular lumen.2,6,7 Histological studies from autopsies in men who underwent haemodialysis or peritoneal dialysis showed epithelium columnar transformation with occasional papillary proliferations without finding evidence of atypia or mitoses. In our study, we also identified hydrocoele and inguinal hernia repair as possible causes, likely due to pressure exerted upon the testicular cord.
Despite malignant transformation of the rete testis being rare, some past literature has referred to it, always acknowledging the rarity of this degeneration.8 Since the bulk of the evidence suggests that TERT is a condition with benign behaviour, a correct differential diagnosis is the most important aspect of the disease. In the presence of a cystic image in the mediastinum testis, it is important to know the features that allow us to distinguish between the different possible diagnoses. Intratesticular varicocoele has ultrasound characteristics that are very similar in terms of morphology and location to those of TERT. However, the two conditions can be clearly distinguished using Doppler ultrasound sonography, which reveals a slow vascular flow in cases of varicocoele, a finding that is absent in tubular ectasia. This flow is more obvious during a Valsalva manoeuvre or in the standing position. Intratesticular varicosities usually appear in patients with extratesticular varicocoele. In addition, a hypotrophic ipsilateral testis may be observed, which can manifest as testicular asymmetry.9,10
Another similar condition which simulates TERT is cystic dysplasia. Cystic dysplasia typically appears in the paediatric population, with a mean age of 5.8 years at presentation.11 It was first described by Leissring and Oppenheimer.12 When cystic dysplasia is detected, a radiologic evaluation of the upper urinary tract should be performed because its presentation is usually associated with other urological anomalies. Multiple treatment options have been proposed from orchiectomy to cyst excision. As the lesion is benign and malignant degeneration has never been reported, conservative management may be an option.13
Cysts of the tunica albuginea are small anechoic nodules generally located within the superficial testicular layers, and show no flow signal in Doppler exploration. Furthermore, these lesions are palpable at physical examination and are commonly discovered by the patient; they are usually described as a painless nodule <5 mm. Detection of these cysts may follow a haemorrhage, trauma, or infection of the cyst. Most cases require no subsequent treatment measures.14
Lastly, it is essential to distinguish TERT from testicular tumours, especially in cases where cystic formations are common, for example in patients presenting with testicular teratoma.4 Age may offer distinguishing information, with testicular tumours affecting more young men than TERT. These patients usually consult for a hard testicular nodule or an increase in the diameter of a testis. A key ultrasound feature in these cases is increased blood flow around the testicular tumour cyst upon Doppler exploration. This usually corresponds to the proliferative state of tumour tissue surrounding a cyst. Cysts can present as multi-septum, heterogeneous, expansive lesions, and may be observed in the interpolar region of the testicle. Microlithiasis may also be observed inside or nearby the lesion.15,16 In the event of diagnostic doubt following SU, serum β-human chorionic gonadotropin, α-fetoprotein, and lactate dehydrogenase testing should be performed, as well as a genital and pelvic MRI study. One patient in our series was previously affected by contralateral seminoma (20 years ago); the subsequent follow-up includes monitoring of serum tumour markers, SU, and chest X-rays performed on an annual basis. No malignant transformation of the lesions was observed in our series of cases and it is an uncommon condition in the reviewed literature.
None of our patients presented with bilateral lesions, probably due to having local and unilateral findings on SU and associated conditions, which are probable causes of TERT. No conditions with the potential to affect both testes, such as vasectomy or systemic diseases, were observed in our series. No treatment measures are required following the diagnosis, and no subsequent serial imaging controls are usually needed.1,2,17
CONCLUSION
TERT is a condition typically found in men >50 years of age. It tends to be an incidental finding in the context of SU exploration performed for other reasons. Imaging appears very typical, though the differential diagnosis is comprised of a range of conditions that include testicular tumours with a cystic component as a worrying possibility. However, few cases of malignant transformation have been found in the reviewed literature. Consequently, follow-up or treatment is usually not necessary, provided a firm diagnosis has been established.








