Abstract
Bladder cancer is a worldwide health problem, due to both its high prevalence and the cost related to the treatment. It is usually identified on the basis of visible blood in the urine or blood found on urine testing, but emergency admission is a common way for bladder cancer to present and is often associated with a poor prognosis. The contracted bladder is a rare and serious complication which is disabling. In these cases, there is a need for a neobladder, which may lead to voiding dysfunction. Physiotherapeutic avenues have demonstrated effectiveness in the treatment of voiding dysfunction; they rehabilitate the individual and improve their quality of life. This study reports the case of a male patient who underwent transurethral resection of a bladder tumour (high-grade T1 carcinoma), which developed complications during treatment with Bacillus Calmette-Guérin. He also underwent cystoprostatectomy with ileal orthotopic neobladder.
CONTEXT
Bladder cancer is a public health problem. In 2012, it was the ninth most common malignant neoplasia in the world. It has a high prevalence in several populations and its treatment has a high cost.1,2 The American Cancer Society (ACS) estimated there would be 81,190 new cases of bladder cancer, 62,380 cases related to men and 18,810 to women, in the USA during 2018.3
With regard to Europe, in 2012 it was estimated there were 118,000 new cases and 52,000 deaths. Expenditures have been estimated at around €4.9 billion in the European Union (EU).4 The majority (90%) of cases of bladder cancer are urothelial carcinoma in Western Europe and in the USA. Squamous cell bladder cancer is more common in Africa, where schistosomiasis infections are more prevalent. Recent studies have shown that the USA and Western Europe reported particularly high incidence rates, while countries in Eastern Europe and Asia have the lowest rates.4
According to the Instituto Nacional de Câncer (National Cancer Institute, INCA), approximately 9,480 cases of bladder cancer were expected in Brazil during 2018: 6,690 cases in men and 2,790 in women.4 There are risk factors associated with the development of bladder cancer, such as age and race, with elderly white men being the group most likely to develop this type of cancer. Smoking can increase the risk of developing bladder cancer. Another risk factor is exposure to various chemical compounds.5 Of these cases, 75–85% are composed of non-muscle invasive tumours, meaning that the disease remains confined to the mucosa (Ta-CIS) or to the submucosa (T1); patients with this condition are potential candidates for complementary therapy with intravesical chemotherapy or immunotherapy.1,6,7
Since the introduction of intravesical immunotherapy using Bacillus Calmette–Guérin (BCG) as an adjuvant to treatment, a decrease in the rate of recurrence has been reported.8 Although the use of BCG is considered to be effective, not all cases benefit from this treatment. Toxicity, varied complications, and lack of therapeutic response should be taken into account when proposing adjuvancy.9,10
The most common complications are easily resolved, but the contracted bladder is a rare and serious local complication which incapacitates the patient. It is mainly observed in individuals taking part in maintenance programmes.10
In refractory cases or with disabling symptoms, the indication is for cystoprostatectomy with reconstruction of intestinal neobladder. In some cases, after the neobladder reconstruction there is a need for auto-catheterisation, due to the difficulty of emptying and to the presence of urinary incontinence, nocturia, and enuresis.9,10
The incidence of incontinence after this surgery is reported as 30–60% and it is considered an adverse outcome. The incidence of urinary incontinence after orthotopic neobladder is related to the postoperative evaluation time, age of patients, method of surgery, and whether there is intraoperative preservation of nerves.11 Therapeutic options have been limited to date and they include pharmacological treatment, surgical intervention, and pelvic floor physiotherapy.12,13 Physiotherapeutic options are effective in the treatment of voiding dysfunction, which leads to rehabilitation and improved quality of life for the patient.14
CASE REPORT
This case report is a continuation of a previous case reported by Filho et al.2 after follow-up by the pelvic urology and physiotherapy team. A 53-year-old male patient, who was a smoker, with no previous background, presented with painless macroscopic haematuria, which began 3 days before admission to the emergency department in 2009. He underwent ultrasonography of the urinary tract, which revealed an intravesical tumour on the left lateral wall.
Transurethral resection of the bladder tumour with a diagnosis of high-grade T1 urothelial carcinoma was performed. After 8 weeks, the patient underwent a new transurethral resection, this time without relapse or new lesions. Biopsies of the previously resected bed revealed cystitis. He started intravesical adjuvant therapy with BCG (Mycobacterium Bovis BCG, Ataulpho de Paiva Foundation, Rio de Janeiro, Brazil) after 1 month of the last surgical approach, with a total duration of 3 years. The total duration of the treatment followed the protocol of the service, with the induction phase performed for 8 weeks and the maintenance phase for 3 years (1 weekly cycle for 3 weeks, at 3 and 6 months, and every 6 months thereafter), both with a dose of 80 mg at each session.
In the second year of treatment, the patient did not relapse but had some symptoms of the lower urinary tract related to storage, such as frequent urination and voiding urgency without leakage. Despite this, he did not experience a significant deterioration in quality of life.
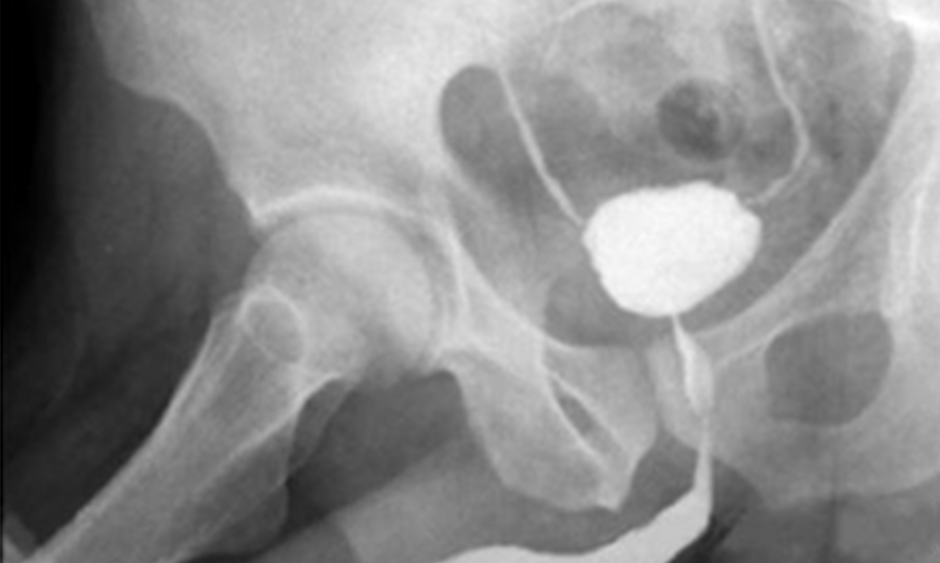
At the beginning of the third and last year of treatment, the urinary symptoms worsened, with an increase in urinary frequency (around 20 times a day), urgency with incapacitating urinary leakage, and suprapubic pain at any bladder filling. During this time, it was necessary to stop the treatment. Urethrocystography revealed a small capacity bladder, bilateral vesicoureteral reflux (degree I), and considerable post-voiding residue (Figure 1).

Figure 1: Image of urethrocystography in the third year of follow-up (maintenance phase with Bacillus Calmette-Guérin ) after transurethral resection.
The urodynamic study demonstrated a very low bladder capacity (40 mL) with a very high sensitivity in this volume and high detrusor pressure (Pdet: 78cmH2O), which confirmed the case of contracted bladder. The cystoscopy of this period showed no neoplastic lesion; however, due to the incapacitating symptoms, the patient underwent cystoprostatectomy, ileal orthotopic neobladder, and lymphadenectomy.
In the intraoperative period, small bladder was evident with no other characteristics. The surgical procedure was uneventful. The patient evolved with ileal loop urinary fistula on the tenth postoperative day, with resolution based on conservative measures. With no other complications, he was discharged from hospital. He was followed up as an outpatient in a neobladder distension programme (Figure 2).

Figure 2: Image of urethrocistography while the patient was in an outpatient clinic undergoing a neobladder distension programme (late postoperative).
After 45 days, the patient presented with repetitive urinary leakage, nocturia, enuresis, absence of voiding desire, and increased urinary frequency, with daily use of four diapers. He was then referred to the pelvic physiotherapy team. Pelvic physiotherapy is considered the first indication of conservative treatment, level A, for pelvic floor dysfunctions involving micturition dysfunction.15,16
The patient had their pelvic-floor muscle function evaluated, which revealed a pelvic-floor muscle function of 1 (scale 0–5), pelvic floor muscles hypotonia, diurnal voiding (performed for 3 consecutive days) with a daytime frequency of 26 times per day, 18 losses per day, and 45g loss on the 1-hour pad test. A total of 12 physiotherapy sessions were performed twice a week with a duration of 1 hour per session. The resources used were anal intracavitary electrostimulation, with a frequency of 3,550 Hz, pulse width of 400–700 μs, and an intensity based on the observation of palpable or visible contractions that were comfortable for the patient; perineal exercises (performed in an outpatient setting and orientated to the home environment); behavioural re-education; and programmed micturition.
The perineal exercises were performed in 3 sets of 10 contractions sustained for 3 seconds, with a rest of 6 seconds, and 10 fast contractions 3 times a day. The behavioural re-education depended on the change of habits, i.e., water intake and toilet habits. The programmed micturition was adjusted every 2 hours initially and then every 3 hours during the day; during the night, 2 micturitions were programmed.
At the end of the sessions, the patient was reassessed. He was first followed-up for 3 months after the sessions and then after 4 years (Table 1).
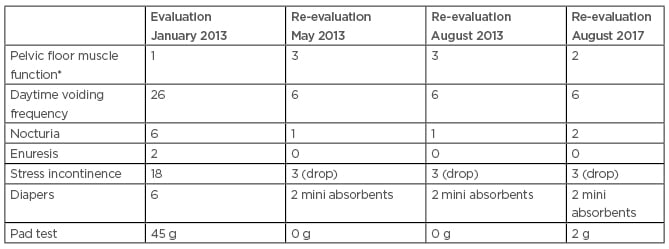
Table 1: Score of the variables observed in the evaluation, reassessment, evaluation at 3 months, and evaluation at 4 years after the physiotherapeutic treatment.
*The modified Oxford scale was used to evaluate pelvic floor muscle function.
FINAL CONSIDERATIONS
The contracted bladder, which is an uncommon complication but one of the most serious, occurs in <1% of individuals.1,8 This complication should be suspected in patients with intense urinary symptoms at any stage and especially in the maintenance of BCG immunotherapy.7,10 In the present study, the first case of bladder contraction in a patient during the combined therapy of the authors’ service was described.9 He evolved to cystoprostatectomy with reconstruction of intestinal neobladder, which resulted in voiding dysfunction.
Reports of voiding dysfunction as a consequence of neobladder have been present in the scientific literature for some years. Hautmann et al.17 followed 211 men for 3 years undergoing reconstruction of the lower urinary tract by means of the ileal neobladder. In this study, 5.5% of the patients did not present with nocturia and enuresis, 6.0% used daily protection, and the remaining patients presented with mild-to-moderate urinary incontinence.
Urinary incontinence impacts the lives of individuals physically, psychologically, and socially. Patients have physical limitations, changes in social and occupational activities, influences on their emotional state and sexual life, as well as social and hygienic discomfort, fear of urinary loss, the smell of urine, the need to use protectors, and the need to change clothes more frequently.18 Nocturia can often disrupt sleep and lead to fatigue, depression, and social isolation.19 In the present case, the patient initially had a voiding frequency of 26 times per day and nocturia 6 times per night, leading to the withdrawal of his professional and social life. He presented with altered sleep and mood.
Mateo et al.20 verified postoperative voiding continence between open and laparoscopic surgery in radical cystectomy with ileal orthotopic neobladder. Of the 72 patients operated on, 4 required auto-catheterisation, 1 underwent open surgery, and 3 underwent laparoscopy. Regarding urinary incontinence, 6 patients from the open surgery, and 11 from the laparoscopy evolved with urinary incontinence. In the present case, the patient presented with stress incontinence, enuresis, and nocturia, without the need for auto-catheterisation. With pelvic physiotherapy, there was a significant improvement of the urinary symptoms over the short, medium, and long-term, as shown in Table 1.
Pelvic physiotherapy is the first-line conservative treatment for voiding dysfunctions, as in the case of urinary incontinence.21 It is a non-invasive, low-cost resource with few contraindications. In the literature, studies about voiding dysfunctions and the use of physiotherapy after surgical correction with cystoprostatectomy and ileal neobladder are scarce. Therefore, further studies are needed to verify the importance of pelvic physiotherapy in such dysfunctions. The success of the physiotherapeutic approach in the present case report is highlighted.
CONCLUSION
The physiotherapeutic intervention in voiding dysfunction after ileal neobladder was effective as a treatment in the reported case, improving the quality of life of the patient. However, the authors suggest that new studies should be carried out with larger series of cases from different centres to compare with these results.