Abstract
Fracture of the penis is not uncommon and usually occurs during intercourse when the erect penis forcefully hits against the perineum or symphysis pubis. The aetiology varies with geographical area, and additionally penile self-manipulation is more common in the Middle East. While imaging may be used as an adjunct to aid diagnosis, especially in equivocal cases, it remains largely a clinical diagnosis. Immediate repair has been established as the standard of care although delayed repair has also been employed with equally successful outcomes. The degloving incision facilitates very good exposure but repair may be undertaken via a simple direct incision if the fracture site can be localised. Urethral injuries usually require repair, although successful non-operative management of small partial tears has been described. Postoperative medications to suppress erections have not been of proven benefit.
Penile fracture may be defined as traumatic disruption of the tunica albuginea and enclosed corpus cavernosum as a result of blunt trauma to the erect penis. It may involve the corpus spongiosum and the urethra.1,2 The aetiology of penile fracture varies with geographical area. In the Western hemisphere vaginal intercourse accounts for most cases of penile fracture.3 Reports from Japan indicate that only 19% of their cases result from sexual intercourse, with other aetiologic factors being masturbation and rolling over in bed onto an erect penis. Penile fracture during intercourse occurs as the result of the erect penis forcefully hitting against the perineum or symphysis pubis. In one large series from the Middle East, more than three-quarters of the reported cases of fractured penis were as a result of manually bending the erect penis to achieve detumescence, a practice known as Taqaandan.4 However, in another Iranian study of 620 men, most cases (56%) were due to sexual intercourse, followed by non-intercourse trauma and masturbation in 24% and 17%, respectively.5 Other much rarer causes of penile fractures include placing the erect penis in tight clothing, falling from a height onto the penis, animal bites of the erect penis, and entrapment of the erect penis in bamboo beds, although the veracity of these accounts can never be verified.6-8
The tunica albuginea is a tough fascial layer which envelops the penis. One of the toughest fascias, the albuginea is normally about 2 mm thick but thins out during erection to about 0.25–0.50 mm and loses its elasticity.9 It has been estimated that the intracorporeal pressure required to rupture the tunica is in the region of 1,500 mmHg, which far exceeds the 100 mmHg that is the normal intracorporeal pressure during an erection.10 During acute loading, usually via angulation of the erect penis, the intracavernous pressure may increase to such an extent as to cause rupture of the tunica. Cavernosal blood leaks into surrounding tissues and may remain confined to the penis if Buck’s fascia is intact or, if Buck’s fascia is ruptured, blood extravasates around Colles’ fascia creating a ‘butterfly’ ecchymosis in the scrotum and perineum.11
Albugineal rupture is mostly unilateral, transverse, and proximal, and usually occurs ventrally in coital-related injuries.3,12 Tears more commonly (75%) affect the right side9 and bilateral corporal tears occur in 4–14% of patients.7,13 Urethral injury seems to be diagnosed more commonly in the USA and Europe (20–38%) compared to Asia (0–3%) and the likelihood of a urethral injury is increased in cases of bilateral corporal tears.11,12
Penile fracture is largely a clinical diagnosis based on history and physical examination and the diagnosis is usually readily made based on clinical features.11 At the time of injury, the man usually reports hearing a cracking sound. Immediate detumescence and pain usually follows.3 Acute swelling and penile deformity may give rise to the ‘eggplant’ or ‘aubergine’ sign.9 If Buck’s fascia is intact, the underlying clot over the fracture site may be palpated as a discrete swelling over which the penile skin can be rolled giving rise to the ‘rolling sign.’ This sign may be elicited in the acute setting as originally described by Naraynsingh and Raju.14 but may be particularly well illustrated in delayed presentations with resolution of the surrounding oedema.14,15 Due to the mass effect of the haematoma, the penis may be deviated to the contralateral side.12 Gross or microscopic haematuria, blood at the meatus, or difficulty voiding may be indicative of urethral injury, but this cannot be ruled out in their absence.16
In most cases the diagnosis of fractured penis can be made clinically without the need for further investigations,17 but some studies may be necessary in equivocal cases or specific clinical scenarios. Urinalysis should be undertaken to assess for microscopic haematuria, which may be a marker of a non-apparent urethral injury, bearing in mind that it may have a positive predictive value of around 50%.7 Ultrasonography may detect tunical defects or haematomas and has a sensitivity of around 86% but remains very operator-dependent.18 It is however readily available and non-invasive. An ultrasonographic grading system for these injuries has been proposed by Shukla et al.19 to assist in the planning of surgical management. The grades range from 0–4, with Grade 0 denoting a normal tunica albuginea. Grade 1 injury represents a defect in the tunica albuginea with cavernosa involvement, Grade 2 demonstrates a haematoma in the subcutaneous tissue as well as in the corpora cavernosa, and Grade 3 suggests a more severe injury with deep fascial haematoma and involvement of the corpora spongiosum. Grade 4 injury implies urethral and vascular involvement with vascular malformation.19
Retrograde urethrography may be conducted in cases where urethral injury is suspected but is not always readily available.20 Cavernosography may also be used to localise the albugineal tear and may prove useful in certain clinical scenarios, for example in the case of a suspected fracture when none can be found intraoperatively.9 It is also not without risk, as side effects include corporal fibrosis, priapism, and contrast reactions.21,22 MRI is an accurate modality in the imaging of penile fracture which could potentially aid localisation of the tunical rupture,23 but it is limited by cost and availability. Practically, intraoperative flexible cystoscopy may be done at the time of repair when a urethral injury is suspected and costs little by way of time and morbidity.5
Penile fractures have been managed conservatively in the past. Conservative measures have included pressure dressings, cold compresses, and anti-inflammatory drugs. Conservative management has lost favour because of the high rate of complications compared to immediate surgical repair, including infected haematoma, abscess, erectile dysfunction, penile curvature, and arteriovenous fistula. In addition, these patients may have prolonged hospitalisation (as long as 2 weeks).24 In a 22-year review of 29 patients, 12 treated with immediate surgery and 17 with conservative management, Muentener et al.25 noted a significantly higher rate of complications in the conservatively treated group. The surgically managed patients were more likely (92% versus 59%) to have a good outcome. This has led to the adoption of immediate repair as the standard of care in penile fractures.5,9
Most authors, as discussed, advocate early repair of penile fractures. This is not, however, the only approach, and a case may certainly be made for a late delayed repair, which should not be confused with the conservative management mentioned above. During the early period following injury, extensive soft tissue oedema makes clinical identification of the injury site difficult and full exposure would require a circumcising degloving incision. Such extensive dissection has been associated with complications such as skin necrosis and sepsis in as many as 66% of patients.26 If presentation is delayed by several days, tissues may in fact still be friable, making repair more difficult. Naraynsingh et al.15 note that a 7–12 day waiting period allows resolution of tissue oedema. Since most of the clot is trapped by Buck’s fascia and is localised to the site of injury, the swelling resolves much less quickly at the site of the fracture. This produces a well circumscribed swelling over the fracture site over which the overlying skin may be rolled and has been termed the ‘rolling sign’ (Figure 1).

Figure 1: Delayed repair often allows localisation of the fracture site, seen here as a swelling on the shaft.
By allowing resolution of tissue oedema the fracture may be accurately localised and repaired via a small direct incision as discussed below.15 In a seminal prospective study, Nasser and Mostafa27 reported on late delayed repair among 24 men presenting late (>24 hours) following penile fracture. In this series, patients underwent conservative treatment for 7–12 days following which surgical repair of their fractures was carried out under local anaesthesia. The authors reported excellent outcomes, with all patients regaining sexual function at 4–6 weeks.27 Appropriate patient selection is key however, as the patient should have no urethral injury. One retrospective study did note an increased rate of erectile dysfunction among patients undergoing delayed repair, with Bozzini et al.28 noting worse outcomes among men operated on after 8.23 hours compared with before 8.23 hours. However, a recent systematic review of 12 studies involving 502 patients reported no difference in erectile dysfunction or scar formation between immediate and delayed repair.29 The authors have employed this delayed technique to good effect.
Numerous incisions have been used, among them the circumcising degloving, inguinoscrotal, midline penoscrotal, and lateral incisions.11 The circumferential degloving incision has gained popularity among many surgeons. Ozcan et al.30 cite the fact that in up to 38% of cases there is an adjacent urethral rupture, arguing that a degloving incision allows adequate examination of the corpus spongiosum and avoids missing a urethral injury. They also point to the benefits of good exposure in cases in which there is rupture of the dorsal vein without corporeal injury. The subcoronal approach is associated with a reduced risk of scarring as compared to longitudinal incisions.30 The penoscrotal incision also affords excellent access to the proximal penis, which is more commonly the site of injury. This incision avoids degloving, which is sometimes challenging in a swollen penis, and may be extended as necessary. Mazaris et al.31 described the successful application of this incision among eight patients undergoing immediate repair. The penoscrotal incision may also be used in cases of delayed repair.32
There are, however, other choices of incision. Naraynsingh et al.15,33 have advocated in several publications repair via a small localised incision over the site of injury. This localised incision lends itself to a same day procedure under local anaesthesia and involves much less dissection, and by extension potentially less trauma, to neurovascular structures. The same authors have used a simple direct incision technique in both the acute and delayed repair once they were clinically able to localise the fracture site. This has subsequently been validated as safe and effective in a larger series of patients who underwent delayed repair.27 Proponents suggest that a localised incision may avoid the potential complications of a general or regional anaesthesia as well as those associated with a degloving incision such as abscess, wound infection, or subcoronal skin necrosis.26
Regardless of choice of incision, the principles of repair as are follows:9
- Exposure
- Evacuation of the haematoma
- Identification of the site of fracture (Figure 2)
- Wound toilet and freshening of the tunical edges (Figure 3)
- Suturing of tears in the tunica albuginea
- Restoration of the urethral integrity
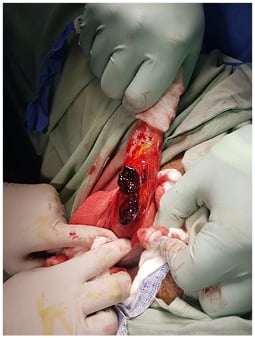
Figure 2: Degloving incision and identification of the fracture site.

Figure 3: Evacuation of clot and freshening of tunical edges prior to closure.
Naraynsingh and Raju recommend closure with running or interrupted absorbable sutures.14 In contrast, some authors favour non-absorbable sutures, citing the fact that they hold the tunical edges together for a long time even in the face of varied intracorporeal pressure changes. However, foreign body granulomas, stitch sinus, and palpable knots may complicate the use of non-absorbable sutures. The problem of palpable knots may be circumvented by inverting the knots.34 Practically speaking, the authors have used a range of different sutures with equally satisfactory results although our preference is for absorbable materials, such as polydiaxanone or poliglecaprone, using a running stitch.
Management of urethral injuries deserves special mention. Partial tears may be managed successfully by urethral catheterisation, closure over a urethral catheter, or suprapubic cystostomy.9,35 While it has been traditionally advised that complete urethral ruptures be additionally diverted via a suprapubic cystostomy, Singh36 advises that such diversion should only be offered to complex cases with wide distraction defects or when significant sepsis precludes primary urethroplasty. Corporal-urethral fistulae have been reported due to the proximity of the corporal and urethral repairs37 and the development of a sub-Dartos flap with interposition between the corporal and urethral repairs has been described in the literature.11,16 For urethral repair, the authors would recommend absorbable suture material. The authors’ choice of suture is poliglecaprone (Monocryl). It should be noted that non-operative management of urethral injuries has been described.35 In cases where the patient is able to void spontaneously, and in which there is free flow of contrast past the lesion, the authors suggest observation, citing the potential for stricture formation which may follow urethral repair.
Opinion is divided on the use of a perioperative urethral catheter. Some authors recommend routine catheterisation at the time of surgery as this not only aids dissection but facilitates easy urethral repair in the event of a tear.11,38 Others have used it when injuries were close to the urethra.6 When there is a urethral injury and a catheter is used to scaffold the repair it should be kept in place for 7–10 days.11 Early erections following surgery are a concern as this has been associated with dehiscence of the corporal repair.38 A number of medications, such as antiandrogens or sedatives, have been used to suppress erections and some recent publications still advocate their use.2 However, it has been argued that these may be unnecessary because postoperative pain is likely to prevent rigid erections and indeed this issue did not arise in any of the authors’ cases.11 While some authors have recommended as much as a 6-week period of abstinence,21 Uygur et al.39 reported no recurrences among 32 patients, a significant number of whom resumed intercourse at two weeks.
Surgical repair of penile fractures is advocated by the majority of investigators to diminish the incidence of fracture complications, but even this approach has its attendant sequelae. Several recent series have quoted incidence rates of postoperative complications to be around 6–25%. The most frequent complications after surgical repair of the fractured penis are painful erection and intercourse, penile deformity or deviation, skin necrosis, erectile dysfunction, and urethral strictures.2 Zargooshi4 reported excellent sexual function among >300 patients who underwent repair.
Occasionally, other conditions may masquerade as penile fractures and are treated as such, resulting in negative penile explorations. The most frequent mimics are dorsal arterial and venous ruptures, which are often only distinguishable from corporal injury by cavernosography.40,41 Traumatic intercourse may also result in penile suspensory ligament rupture, with a presenting history similar to that of penile fractures, but the examination finding of a floppy penis is usually the discerning feature.42 Among 86 patients, Moslemi43 noted that almost all were able to attain good erections but did note a 2.3% incidence of penile curvature.
CONCLUSION
Fracture of the penis in the West usually occurs following intercourse, when the erect penis hits the perineum or symphysis pubis. While imaging may be used as an adjunct to aid diagnosis, especially in equivocal cases, it remains largely a clinical diagnosis. Immediate repair has been established as the standard of care, but delayed repair has been employed with equally successful outcomes. The degloving incision facilitates very good exposure but repair may be undertaken via a simple direct incision if the fracture site can be localised. Urethral injuries usually require repair although successful non-operative management of small partial tears has been described. Postoperative medications to suppress erections have not been of proven benefit.








