Abstract
Objective: To evaluate whether alpha blockers facilitate the navigation of the ureteroscope through the ureteric orifice, if administered preoperatively, based on the role of alpha blockers, mainly tamsulosin, in medical expulsive therapy of ureteric calculus.
Methods: A prospective, case-control study of 174 patients who underwent ureteroscopic stone removal for lower or mid ureteral calculi between November 2014 and March 2016 was carried out. We included patients >14 years of age who were planned for ureteroscopic stone removal. We divided the patients into two groups, including those who were not prescribed alpha blockers prior to surgery (Group A: no alpha blocker) and those patients who were started on alpha blockers, tamsulosin 0.4 mg, 3 days prior to surgery (Group B: alpha blocker). We excluded patients with stone size >1 cm, spontaneous stone passage prior to surgery, unable to perform ureteroscopy (URS), and previous history of ureteroscopic intervention.
Results: Our study included 124 patients, among whom 60 patients were prescribed alpha blockers preoperatively (Group B). The mean age of the study population was 37.62+9.74 (15–64 years) and the mean stone burden was 38.92+8.21 (15.94–58.12 mm2). The difference in rate of ureteroscope negotiation through the ureteric orifice between Groups A and B was not statistically significant (p=0.57).
Conclusions: In URS, preoperative administration of alpha blockers failed to improve technical ease and lower complication rate. Further large group, multi-centre studies are required todiscover a definitive role of alpha blockers prior to URS.
INTRODUCTION
5–8% in Europe, and 1–5% in Asia.1 Urolithiasis is one of the most common reasons for frequent Urolithiasis is a worldwide public health problem. visits to hospital emergency departments. Ureteral The estimated prevalence is 8–13% in the USA, stones are the leading cause of colicky pain and the majority of these pass spontaneously. In the literature, it has been reported that ~70% of ureteral calculi were located in the lower third part of the urinary tract.2 Medical expulsive therapy (MET) is recommended by the European Association of Urology (EAU) (2013) for 5–10 mm ureteric stones to facilitate stone passage. For MET, alpha blockers, mainly tamsulosin, have shown efficacy in several randomised controlled trials.3-5 The underlying pathophysiology of this therapy is supported by the presence and distribution of adrenoreceptors in the ureter; alpha-1D and alpha-1A are the most common adrenoreceptors, and are more numerous in the distal ureter.6 Blocking the action of alpha-1 receptors by pharmacological agents (alpha blockers), such as alfuzosin, terazosin, doxazosin, and, most typically, tamsulosin, results in the relaxation of the ureteric smooth muscle.7-9
Ureteroscopy (URS) is the most commonly performed procedure for the treatment of ureteral calculi, with a high (>90%) stone-free rate after a single treatment. Technical advancements in the armamentarium of semi-rigid URS, including the design and miniaturisation of scopes and availability of the Holmium:YAG laser, ensures a precise and excellent safety profile with a powerful stone fragmentation mechanism.10 Difficulty in negotiating a ureteroscope or ureteral access sheath through the vesico-ureteral junction is a common occurrence. Surgeons advocate various strategies to facilitate the passage of ureteroscope or ureteral access sheath for performing URS or retrograde intrarenal surgery. Routine preoperative stenting has been recommended by some authors to facilitate passive ureteral dilatation.11
Based on the role of alpha blockers, mainly tamsulosin, in MET of ureteric calculus, we attempted to extend the use of alpha blockers prior to URS for procedural ease. We conducted a prospective, case-controlled study to evaluate whether alpha blockers facilitate the negotiation of the ureteroscope if administered preoperatively.
MATERIALS AND METHODS
Study Design
We conducted a prospective, case-controlled study of 174 patients at the Urology Department, King George’s Medical University, Lucknow, Uttar Pradesh, India, who underwent ureteroscopic stone removal for lower or mid-ureteric calculi between November 2014 and March 2016. We included patients >14 years of age who were planned for ureteroscopic stone removal. We divided the patients into two groups: those who were not prescribed alpha blockers prior to surgery (Group A: no alpha blocker [NAB]) and those patients who were started on alpha blocker tamsulosin 0.4 mg, 3 days prior to surgery (to decrease the chances of under dosing and to achieve optimum serum level) (Group B: alpha blocker [AB]). We excluded patients with stone size >1 cm, spontaneous stone passage prior to surgery, those who could not have URS performed, patients with ureteral strictures and ureteral anomalies, and previous history of ureteroscopic intervention. Eighteen patients were excluded from the study due to consent withdrawal (5 patients), spontaneous stone passage (2 patients), and failure to perform the procedure (procedure was abandoned due to inaccessible ureteric orifice) (11 patients). Patients were divided into either the NAB group or AB group (Figure 1).
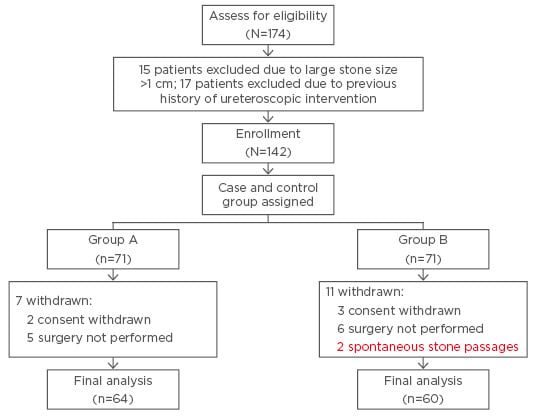
Figure 1: Schematic diagram showing study design.
Operative Technique
At our centre, semi-rigid URS (6.5/8.5 French scale [Fr], Wolf, Richard Wolf Medical Instruments Corporation, Illinois, USA) is performed by standard technique by experienced urologists, all senior residents and faculty of the department, and under regional or general anaesthesia. No significant difference in anaesthesia technique was made between the two groups. Operative time was calculated from insertion of the ureteroscope per urethra to ureteroscope removal after stone removal. The ureteric orifice was dilated with the help of a balloon dilator (8 Fr), ≤14 atmospheric pressure for 2 minutes under direct vision with a 22 Fr cystoscope, if required. Stone fragmentation was performed either using a holmium laser (365 nm fibre, Auriga holmium laser system, StarMedTec GmbH, Starnberg, Germany) or pneumatic lithotripter, based on the surgeon’s preference or availability of equipment. Fragments of stone were removed with the help of removal forceps. On completion of the procedure, we placed the 5/6 Fr double J stent under fluoroscopy (Siemens Multimobil 5E system, Siemens Healthcare GmbH, Erlangen, Germany) in selected cases. Foley catheter was removed on postoperative Day 1. Postoperative clearance was checked by imaging, including x-ray KUB or USG KUB on postoperative Day 1. The double J stent was removed after 1–2 weeks under sedation and antibiotic coverage. All complications were reported by the operating urologist using the Modified Clavien Classification System. A separate grading protocol was used for the patients who had >1 complication, with each one reported separately.
Statistical Analysis
Data analysis was conducted using SPSS Statistics version 16.0 (Chicago, Illinois, USA). The unpaired t-test was used for analysing continuous variables, and categorical or dichotomous variables were evaluated by using the chi-square test. The results were presented as a proportion (%) and mean (+ standard deviation). All p values were two-pronged, with p<0.05 considered statistically significant.
RESULTS
Our final analysis included 124 patients, among whom 60 patients were prescribed alpha blockers preoperatively (Group B). The mean age of the study population was 37.62+9.74 (15–64 years). The mean stone burden was 38.92+8.21 (15.94–58.12 mm2) including 77.42% population with lower ureteric stones. Out of 124 patients, 41 (33.06%) patients did not require vesico-ureteric junction dilatation for ureteroscope insertion and 60.98% were prescribed alpha blockers preoperatively. The difference in the rate of ureteroscope negotiation through the vesico-ureteric junction between the NAB and AB groups was not statistically significant (p=0.57) (Table 1).
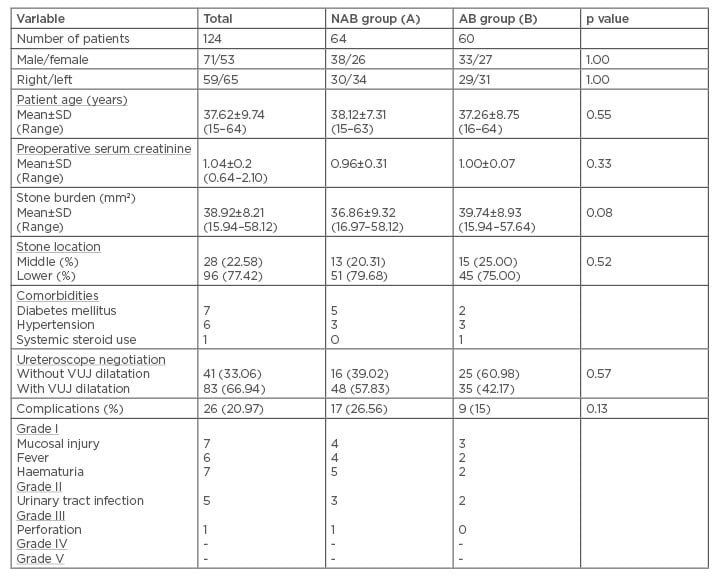
Table 1: Pre and postoperative data of ureteroscopy procedure.
NAB: no alpha blocker; AB: alpha blocker; SD: standard deviation; VUJ: vesico-ureteric junction.
DISCUSSION
In the human ureter, three types of alpha-1 adrenergic receptors are expressed, among which subtype alpha-1D predominates.11 Experimental studies showed that the alpha-1A adrenergic receptor has a key role in ureteral contraction.12,13 Tamsulosin effectively blocked all subtypes of alpha-1 adrenergic receptors and inhibited spontaneous ureteral contractions. In the literature, Level I evidence exists, supporting the role of alpha-1 adrenergic receptor antagonists in conservative management of ureteral stones.14,15 The underlying mechanism of stone expulsion is most likely related to direct inhibition of ureteral contractions and subsequent ureteral relaxation.
Patients with ureteric calculus perceive anxiety about the sudden onset of colicky pain and remain uncertain about spontaneous passage of stones. Several meta-analyses and randomised controlled trials encouraged clinicians to prescribe MET to decrease stone-related symptoms, facilitate and hasten stone passage, and reduce the need for active intervention. In the current scenario, an alpha-blocker (tamsulosin 0.4 mg once daily) and a calcium channel blocker (nifedipine 30 mg once daily) have shown efficacy in the production of desired clinical outcomes in several studies.16,17
Ureteroscopic lithotripsy has emerged as a favoured procedure for ureteric calculus by a urologist, because of the high stone-free rate and immediate symptom alleviation. In cases of difficult ureteral access, the ureteric orifice has to be dilated, either by balloon dilator or similar means. The use of balloon dilators may be associated with significant ureteral injury.18
In our study, we divided and assigned patients based on administration of daily doses of tamsulosin 0.4 mg prior to URS. Out of 124 patients, 33% of patients did not require ureteric orifice dilatation for ureteroscope insertion. Among these 41 (33%) patients, 25 (61%) belonged to Group B in which tamsulosin was started as compared to 16 (39%) from Group A. This difference was statistically insignificant, but clinical application in reducing the need of ureteral dilatation during URS can be appreciated by the operating urologist in reducing operative time and complications. The pathophysiological basis of using alpha blockers in MET for ureteric calculus may have hidden potential which can be applied in other ureteral interventions. Our study is an effort to reveal the effect of alpha blockers on ureteral orifices and the lower ureter, which may facilitate the URS and help to reduce procedural complexities.
Our study is strengthened by being one of the first studies in which pre-URS alpha blockers were used. The limitations of this study included the heterogeneity of surgeon’s experience, lithotripsy (holmium and pneumatic), and anaesthesia (general versus spinal). Moreover, our study is limited by the small number of subjects. To the authors’ best knowledge, no such study is found in the literature. We conducted a prospective, case-controlled study to reduce selection bias.
URS is a safe and effective procedure. In the literature, a complication rate ranging between 3%19 and 30% has been described. Mandal et al.20 studied 120 patients who underwent unstented URS and reported a 30% complication rate. The Modified Clavien Classification System has classified complications in five grades. Grades 1 and 2 are considered as minor and Grades 3–5 as major complications. In our study, we encountered an overall complication rate of 21% (77% minor). No statistically significant difference in complication rate was found between the two groups.
CONCLUSION
Ureteroscopic lithotripsy is a safe and effective procedure for ureteric calculus with the highest stone-free rate and immediate symptom relief. The use of alpha blockers, mainly tamsulosin, is well-proven in MET. In URS, preoperative administration of alpha blockers failed to demonstrate the benefits of technical ease and lower complication rate. Further large group, multi-centric studies are required to find a definitive role for alpha blockers prior to URS.








