Interviewees:
Neil Barber, Keng Lim Ng
Department of Urology, Frimley Park Hospital, Frimley, UK
Disclosures: Barber has been a proctor/speaker for Teleflex, Olympus Keymed, Boston Scientific, Procept Bio-Robotics, and Cambridge Medical Records (CMR). Ng has declared no conflicts of interest.
Acknowledgements: Medical writing assistance provided by Stefan Amisten.
Support: The publication of this article was funded by Teleflex.
Citation: EMJ Urol. 2021;9[1]:63-70.
Interview Summary
Benign prostatic hyperplasia (BPH) is a chronic age-related condition associated with lower urinary tract symptoms (LUTS). Although conservative management and pharmacological treatment is the first choice for the management of LUTS/BPH, a very low adherence to, and satisfaction with, pharmacological management regimens in patients with LUTS/BPH suggests that BPH might frequently be inadequately managed by pharmacological interventions. Both invasive and minimally invasive surgical therapies (MIST) are currently available for the surgical management of BPH not responding to conservative or pharmacological management. The development of novel surgical interventions for the management of BPH is evolving rapidly, and a plethora of different invasive and MIST interventions are now available to treat BPH.
MIST procedures such as the prostatic urethral lift (PUL; utilising the UroLift® System, Teleflex, Pleasanton, California, USA) and Rezum® (Boston Scientific, Marlborough, Massachusetts, USA), have reported low rates of sexual dysfunction relative to transurethral resection of the prostate (TURP), the current gold standard surgical therapy for BPH. The L.I.F.T. pivotal trial for PUL reported no instances of new, sustained erectile or ejaculatory dysfunction, whereas TURP is associated with both erectile dysfunction (0–3% of cases) and ejaculatory dysfunction (5–15% of cases). PUL is currently the only leading MIST that offers rapid, significant, and durable symptom relief of LUTS without causing new, sustained erectile dysfunction or ejaculatory dysfunction.
Recent guidelines issued by the European Association of Urology (EAU), the American Urological Association (AUA), and the UK’s National Institute for Health and Care Excellence (NICE) recommend PUL for the treatment of BPH with prostate volume 30–80 mL (NICE, EAU)/<80g (AUA). The procedure is also recommended for men who wish to preserve male sexual function. Additionally, EAU guidelines state that PUL is the only surgical intervention recommended for males who cannot have surgery under anaesthesia.
In conclusion, the MIST PUL is endorsed by EAU, AUA, UK NICE, and guidelines for patients with BPH with notable recommendation for males who wish to preserve sexual function or who are not able to have surgery under anaesthesia.
INTRODUCTION
BPH is a chronic age-related condition associated with LUTS such as urinary frequency, urgency, and nocturia. BPH affects one-half of all males aged 50–60 years and is estimated to affect 90% of males aged 80 years or above.1 BPH progression may lead to increasingly obstructed voiding, which may significantly impact quality of life (QoL) through sleep loss, reduced productivity, impaired sex life, social isolation, and depression.2
MANAGEMENT OF BENIGn PROSTATIC HYPERPLASIA
Management options for BPH include conservative management, pharmacological treatment, and surgical interventions.3
Conservative Management
Conservative management, such as watchful waiting, behavioural therapy, and dietary modifications, may be suitable for patients with LUTS that are not troubled enough by their symptoms to require pharmacological or surgical intervention.3,4
Pharmacological Treatment
Pharmacological management, either as mono- or combination therapy, primarily involves the use of drugs that either relax the smooth musculature (e.g., α1-adrenoceptor antagonists, muscarinic receptor antagonists and β3 agonists, phosphodiesterase 5 inhibitors) or exert anti-androgen effects to reduce prostate cell proliferation (e.g., 5α-reductase inhibitors).3
Monotherapy options include α1-adrenoceptor antagonists, which are usually considered the first-line pharmacological treatment due to their rapid onset of action, good efficacy, and low rate and severity of adverse events. However, they may not prevent occurrence of urinary retention or the potential future need for surgery.3 5α-reductase inhibitors may reduce the risk of acute urinary retention and need for surgery but, because of their slow onset of action, they are not suitable for short-term use.3 Muscarinic receptor antagonists and β3 agonists may be considered in males with moderate-to-severe LUTS who mainly have bladder storage symptoms.3 Phosphodiesterase 5 inhibitors may be considered in those with moderate-to-severe LUTS with or without erectile dysfunction.3
Combination therapy in the form of an α1-blocker plus a 5α-reductase inhibitor may be considered in individuals with moderate-to-severe LUTS and an increased risk of disease progression. An α1-blocker plus a muscarinic receptor antagonist combination therapy may be considered for patients with moderate-to-severe LUTS if relief of storage symptoms has been insufficient with monotherapy with either drug.3
A very low adherence to, and satisfaction with, pharmacological management regimens in patients with LUTS/BPH suggests that BPH might frequently be inadequately managed by pharmacological interventions.5 In fact, it has been reported that 25–70% of patients managed pharmacologically for BPH are either non-compliant or discontinue pharmacological management altogether because of lack of effectiveness or bothersome side effects such as erectile dysfunction, ejaculatory dysfunction, weakness, fatigue, and dizziness.6,7
Surgical Treatment
Monopolar TURP is considered to be the gold standard reference technique for the surgical management of LUTS/BPH; however, many alternative techniques have recently been developed. Surgical approaches for LUTS/BPH can be broadly classified into five main categories: prostate resection, prostate enucleation, vapourisation, alternative ablative techniques, and non-ablative techniques.3
Surgical procedures for BPH/LUTS are also classified based on their level of invasiveness into invasive surgical therapies (e.g., TURP, simple prostatectomy) or MIST. MIST interventions may be further classified into either thermo-ablative or mechanical.8
MIST procedures include transurethral incision of the prostate (TUIP); thermo-ablative strategies such as transurethral microwave therapy (TUMT), transurethral electrovapourisation of the prostate (TUVP), or transurethral needle ablation; and mechanical strategies such as PUL (utilising the UroLift System) and intraprostatic stents.
Emerging MIST interventions include prostatic artery embolisation; transurethral water vapour therapy (Rezum); other forms of interstitial ablation using transurethral and transperineally delivered laser energy; mechanical therapies such as the temporary implantable nitinol device (iTIND; Olympus Medical Systems, Tokyo, Japan), ClearRing™ (ProArc Medical, Pardes Hanna-Karkur, Israel), ZenFlow Spring® (ZenFlow, San Francisco, California, USA), Butterfly (Butterfly Medical Ltd., Yokneam, Israel), and high-frequency ultrasound (histotripsy).8-12 A summary of key characteristics of different MIST procedures is presented in Table 1.8
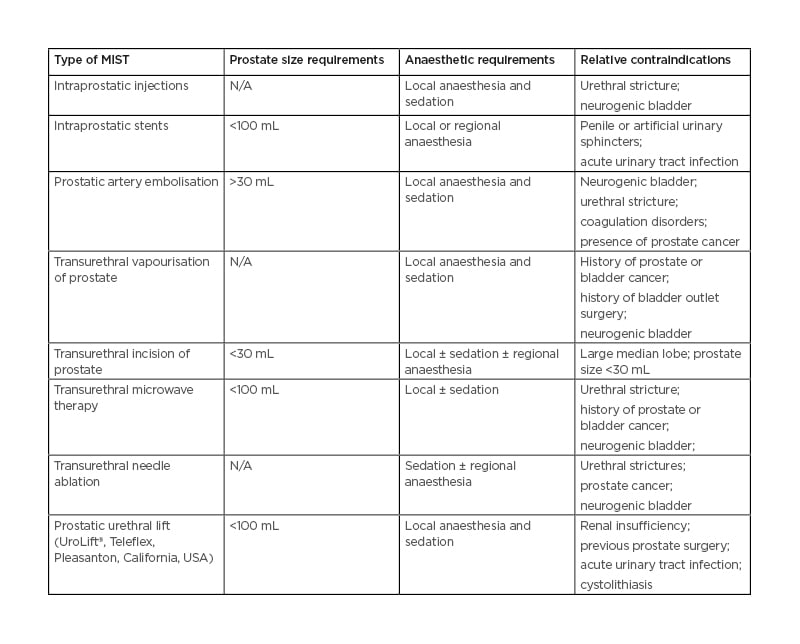
Table 1: Characteristics of different minimally invasive surgical therapy procedures.⁸ MIST: minimally invasive surgical therapy; N/A: not applicable.
CONSIDERATIONS FOR THE SELECTION OF SUITABLE MANAGEMENT SOLUTIONS
Factors influencing the choice of a BPH management solution for an individual patient would include patient evaluation; predicted treatment outcomes achievable by available treatment options; patient preferences; expectations from the chosen treatment option in terms of speed of onset, efficacy, side effects, and QoL; and disease progression.3
Behavioural modification, with or without pharmacological intervention, is usually the first choice of therapy.3 Surgical intervention is most often considered for patients experiencing bladder stones or diverticula; dilatation of the upper urinary tract due to BPO, with or without renal insufficiency; inadequate relief from LUTS or post-void residual urine by means of conservative or pharmacological management; overflow incontinence; recurrent or refractory urinary retention; recurrent urinary tract infections; and treatment-resistant macroscopic haematuria due to BPH.3 Multiple factors, including local surgical expertise, the ability to have anaesthesia, patient preferences, comorbidities, and prostate size, affect the types of surgical interventions that are available for individual patients.3 An individualised, shared decision-making approach is therefore required to determine the ideal treatment option for each patient.13
MINIMISING SEXUAL DYSFUNCTION WITH benign prostatic hyperplasia SURGICAL MANAGEMENT
Sexual activity is an important aspect of many males’ QoL14 and maintenance of sexual function is therefore viewed as a significant attribute by both past and future BPH surgery patients.15 The importance of considering the impact of BPH interventions on male sexual function has therefore resulted in the AUA and EAU now recommending patient sexual health counselling before and after BPH interventions.3,16
Some surgical procedures available for the treatment of BPH are associated with a substantial risk of ejaculatory and erectile dysfunction; TURP is associated with both erectile dysfunction (0–3% of cases) and ejaculatory dysfunction (5–15% of cases).17 However, several MIST procedures have demonstrated encouraging preservation of post-operative sexual function while also providing significant lower urinary tract symptom relief without compromising efficacy and safety.13
Studies on PUL, Rezum, and Aquablation® (PROCEPT BioRobotics, Redwood City, California, USA) have reported lower rates of sexual dysfunction relative to TURP, the current gold standard therapy for BPH.13 In non-head-to-head, indirect comparisons, PUL has been found to be superior to pharmacological therapy in preserving erectile and ejaculatory function and sexual satisfaction in males with BPH.18 These findings are further supported by an indirect comparison using a network meta-analysis model that found that treatment with PUL results in better sexual function domain scores compared to TURP, but not compared to Aquablation.19
Furthermore, controlled studies have reported that both PUL and Rezum preserve erectile function, although de novo instances of ejaculatory dysfunction have been reported with Rezum.20 In contrast, the L.I.F.T. pivotal trial for PUL reported no instances of new, sustained erectile or ejaculatory dysfunction,17 and the PUL procedure is currently the only leading MIST that offers rapid, significant, and durable symptom relief of LUTS without causing new, sustained erectile dysfunction or ejaculatory dysfunction.17,21-24
Prostatic urethral lift IS RECOMMENDED BY CURRENT GUIDELINES FOR SURGICAL MANAGEMENT OF benign prostatic hyperplasia
The EAU, UK NICE, and AUA have all issued guidelines on the surgical management of BPH by both invasive and MIST procedures and endorse the use of PUL of the management of LUTS due to BPH.3,16,25
PUL is the Only Current MIST Strongly Recommended by EAU Guidelines and the Only MIST Mentioned in the EAU Treatment Algorithm for Bothersome LUTS
The EAU guidelines provide algorithms for the conservative, pharmacological, and surgical management of BPH. EAU guidelines also record the quality and the level of evidence available, and derives from that different levels of recommendations of use within described parameters, such as the size of the prostate.3
The EAU guidelines state that factors influencing the choice of treatment include findings from the patient evaluation; the ability of the treatment to change the findings; patient preferences; expectations regarding speed of onset, efficacy, side effects, and QoL; and disease progression. Behavioural modifications, with or without pharmacological treatments, should be considered as the first choice of therapy.3
Surgical intervention is usually required in cases of recurrent or refractory urinary retention, overflow incontinence, recurrent urinary tract infections, bladder stones or diverticula, treatment-resistant macroscopic haematuria due to BPH,or dilatation of the upper urinary tract due to benign prostatic obstruction, with or without renal insufficiency (i.e., absolute operation indications, need for surgery). Additionally, BPH surgery is usually needed when patients have not obtained adequate relief from LUTS or post-void residual urine using conservative or pharmacological treatments (i.e., relative operation indications).3
Prostate size, comorbidities, ability to have anaesthesia, patient preferences, willingness to accept surgery-associated specific side-effects, availability of the surgical armamentarium, and the experience of the surgeon with these surgical techniques are key factors determining the choice of surgical interventions available for the patient.3
EAU presents a surgical treatment algorithm for bothersome LUTS stratified by the patient’s ability to have anaesthesia, the patient’s cardiovascular risk, and the size of the prostate. Current standard/first choice surgical treatment options include TUIP (prostate volume <30 mL); TURP (prostate volume 30–80 mL); open prostatectomy, HoLEP, bipolar enucleation (prostate volume >80 mL); and laser vapourisation.3
PUL is the only MIST to be recommended with a ‘strong’ strength rating for the treatment of LUTS in the EAU guidelines. PUL is the only MIST mentioned in EAU’s treatment algorithm for bothersome LUTS, and is recommended for all patients, regardless of level of risk, for prostate volumes between 30 and 80 mL. The EAU algorithm also positions PUL as the only surgical procedure recommended for patients not able to have surgery under anaesthesia (Figure 1).3
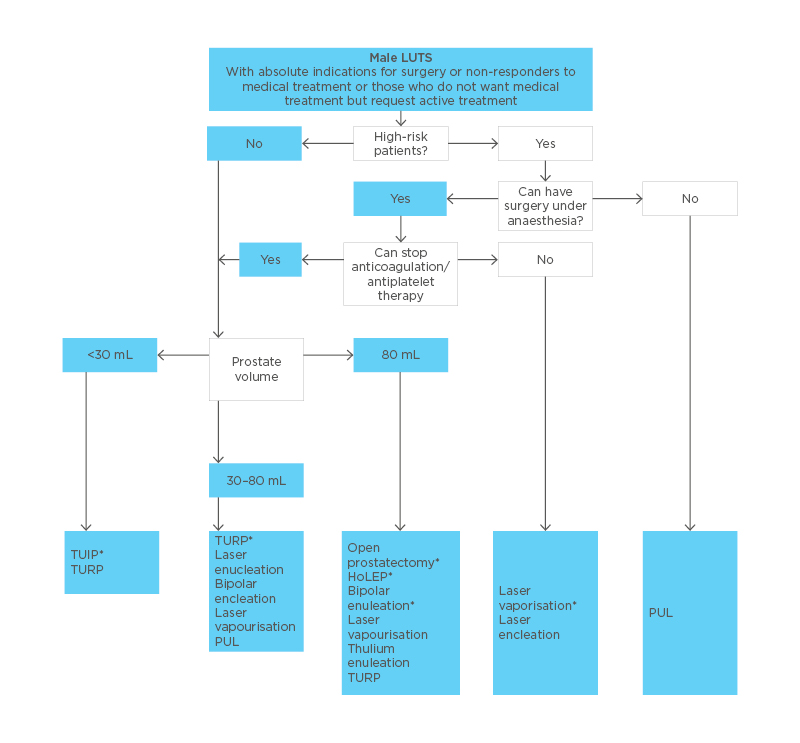
Figure 1: EAU algorithm for the treatment of bothersome lower urinary tract symptoms refractory to conservative/pharmacological treatment or in cases of absolute operation indications.3 *Current standard/first choice.
Alternative treatments are presented in alphabetical order. Laser vapourisation includes GreenLight™ (Boston Scientific, Marlborough, Massachusetts, USA), thulium, and diode laser vaporisation. Laser enucleation includes holmium and thulium laser enucleation. EAU: European Association of Urology; HoLEP: Holmium laser enucleation; LUTS: lower urinary tract symptoms; PUL: prostatic urethral lift; TUIP: transurethral incision of the prostate; TURP: transurethral resection of the prostate.
NICE Recommends PUL for the Management of LUTS Due To BPH
In May 2021, UK’s NICE published guidelines on PUL for the management of LUTS due to BPH.25 NICE recommends PUL for treating LUTS due to BPH, as PUL relieves lower urinary tract symptoms, avoids risk to sexual function, and improves QoL. NICE guidelines also highlight that PUL constitutes a minimally invasive procedure, and that PUL should be considered as an alternative to TURP and HoLEP. The NICE guidance also states that the PUL procedure is suitable as a day-case or outpatient procedure for males aged 50 years and older who have a prostate volume between 30 and 80 mL.
AUA Guidelines Recommend PUL for BPH with Prostate Volume <80 g
The AUA guideline amendment 2019 on the surgical management of LUTS attributed to BPH states that PUL may be offered as an option for patients with LUTS caused by BPH, provided that the prostate size is less than 80 g, and that there is a verified absence of an obstructive middle lobe.16 The AUA guidelines also highlight that PUL or water vapour thermal therapy may be offered to eligible patients who desire preservation of erectile and ejaculatory function (Figure 2).16
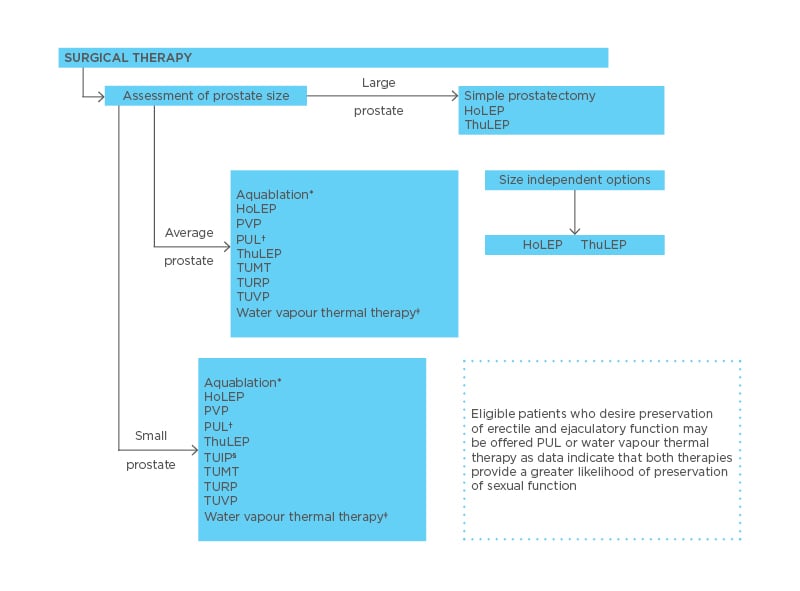
Figure 2: AUA algorithm for the surgical management of lower urinary tract symptoms attributed to benign prostatic hyperplasia.16
*Eligibility for an Aquablation® (PROCEPT BioRobotics, Redwood City, California, USA) procedure is dependent upon prostate volume >30 and <80 g.
†Eligibility for a PUL procedure is dependent upon absence of obstructing midline prostate tissue and prostate volume <80 g. ǂEligibility for a water vapour thermal therapy procedure is dependent upon prostate volume <80 g.
§Eligibility for a TUIP procedure is dependent upon prostate volume <30 g.
AUA: American Urological Association; BPH: benign prostatic hyperplasia; HoLEP: holmium laser enucleation of the prostate; LUTS: lower urinary tract symptoms; PUL: prostatic urethral lift; PVP: photoselective vapourisation of the prostate; ThuLEP: thulium laser enucleation of the prostate; TUIP: transurethral incision of the prostate; TUMT: transurethral microwave therapy; TURP: transurethral resection of the prostate; TUVP: transurethral electrovaporisation of the prostate.
PROSTATIC URETHRAL LIFT GUIDELINE RECOMMENDATIONS ARE SUPPORTED BY A STRONG CLINICAL EVIDENCE BASE
With more than 28 peer-reviewed clinical publications, complemented by real-world evidence studies, PUL is one of the most well-characterised MIST interventions for LUTS/BPH. As a complement to clinical trial data on PUL spanning up to 5 years of follow-up,17 a real world retrospective study of PUL including 3,226 patients across 22 international sites has been conducted.26 Analyses to date suggest that the real world outcomes are largely comparable with the outcomes from previously published PUL clinical studies. 18,24,26,27
CONCLUSIONS
The development of novel surgical interventions for the management of BPH is evolving rapidly, and a plethora of different invasive and MIST interventions are now available to treat BPH. Preservation of sexual function is viewed as an important patient consideration when selecting treatment options for BPH, and interventions such as PUL, Rezum, and Aquablation have reported lower rates of sexual dysfunction relative to TURP, the current gold standard surgical intervention for BPH. With more than 28 peer-reviewed clinical publications, complemented by real world evidence, PUL is one of the most well-characterised MIST interventions for LUTS/BPH, and PUL is currently the only leading MIST that offers rapid, significant, and durable symptom relief of LUTS due to BPH without causing new, sustained erectile dysfunction or ejaculatory dysfunction.
PUL is the only MIST with a ‘strong’ strength rating for the treatment of LUTS in the EAU guidelines, and is the only MIST mentioned in the EAU algorithm for bothersome LUTS. EAU guidelines endorses PUL for the treatment of BPH with prostate volumes between 30 and 80 mL and highlights that PUL is the only surgical intervention recommended for patients not able to have surgery under anaesthesia. Due to its minimally invasive nature and documented preservation of male sexual function, PUL is also recommended by UK NICE and AUA guidelines for BPH with prostate volume not exceeding 80 mL/80 g.








