Abstract
Background: A urethral diverticulum (UD) constitutes a localised saccular dilation that forms out of any point in the urethra’s length, contiguous with the true urethral lumen through an orifice with a variable size neck. Disturbance of urine drainage from this outpouching leads to urinary stasis, recurrent urinary tract infections, lithiasis formation, an increase in UD size, urinary leakage or fistulas, incontinence, or even a palpable penoscrotal mass. UD occurs far more frequently in women and is very rare in men, with the incidence and prevalence in males remaining largely unknown.
Objective: The purpose of this paper is to present an updated review of acquired male UD, according to clinical presentation, diagnostic imaging findings, management, complications, and outcomes.
Material and Methods: Literature searches were conducted using Medline, Embase, and Cochrane databases in June 2015 to identify papers related to acquired male UD, concerning type, aetiology, presentation, radiologic and/or surgical intervention, and outcomes.
Discussion: The most common symptoms are obstructive lower urinary tract symptoms along with haematuria. Additionally, both congenital and acquired diverticula at the penoscrotal angle are frequent. Diagnosis alternates between physical examination and specific imaging, with individualised treatment now being standard practice varying with the location and size of the diverticulum. Besides conservative and observational follow-up, endoscopic and open surgical techniques are the selected definitive management options.
Conclusion: An acquired male UD is rare and must be considered in the differential diagnosis of suspicious penile and scrotal masses. If there is significant urinary stasis, recurrent urinary tract infections, or urethral calculi, a rigorous and thorough clinical examination followed by surgical correction is most often standard procedure, allowing for treatment of symptoms and aetiology simultaneously. Reconstructive urethral surgical corrections are very complex and require a specialised approach, often found only in high-volume surgical centres.
INTRODUCTION
The urethra is a tubular structure with a median length of approximately 17.5–20.0 cm. Its anterior segment stretches from the lower limit of the urogenital diaphragm down to the urethral meatus and can be further divided into bulbar urethra (surrounded by the bulb of the corpus spongiosum) and penile or pendulous urethra (surrounded by corpus spongiosum).1,2 A urethral diverticulum (UD) is a condition in which a localised saccular of fusiform outpouching forms out of any point in the urethra’s length. This saccular dilatation is contiguous with the true urethral lumen through a discrete orifice with a variable size neck. Inadequate urine drainage from this outpouching leads to urinary stasis, recurrent urinary tract infections, lithiasis formation, an increase in UD size, urinary leakage or fistulas, incontinence, or even a palpable penoscrotal mass.3,4
UD occurs far more frequently in women, most likely due to poor anatomical support of the urethra, complications from childbirth, or a more typical occurrence of periurethral abscesses.5,6 UD are estimated to occur in 1–6% of women, presenting usually from the third to the fifth decade of life.6 In men, it is a rare finding, and literature related to male UD generally involves case reports or small patient series with no estimated prevalence reported.1,7
According to Watts,8 UD may be congenital or acquired in origin. Congenital UD are usually associated with congenital anterior urethral valves and aetiologic mechanisms remain to be ascertained: failed attempt of urethral duplication, failure of alignment between proximal and distal urethra, anomaly of the developing urethra resulting in excessive tissue growth and a permanent valve or flap mechanism, and a cystic dilation of periurethral glands.9 These types of diverticula harbour all the layers of the urethral wall and are lined by epithelium. Acquired UD correspond to 67–90% of all male diverticula and is associated with an iatrogenic background, resulting in conditions such as obstructing urethral stricture, blunt trauma, and infection.3 In children, imperforate anus is alsocommon following surgery.3,10 These types of UD are covered by granulation tissue and their walls lack a true smooth muscle layer, only lined by a transitional epithelium and presenting a pseudodiverticulum image.11 Congenital and acquired UD both share the same common feature: blind-ending outpouchings of the urethra.12
Acquired UD in males is a very uncommon and rare condition and the literature associated to it is scarce; as such, its incidence and prevalence remains unknown. It is mostly found at the penile urethra, especially at the penoscrotal angle.13 Several factors have been described as responsible for UD development: strictures; recurrent urinary tract infections, including periurethral suppuration as a result of gonorrhoea, tuberculosis, or chronic urethritis infections; long-term or recurrent catheterisation; urethral or penile surgery; trauma; and erosion from surgical implants or from the use of penile clamps.5,14 Inflammation of the periurethral glands with the formation of abscesses that burst into the urethral lumen has also been reported. Any of these risk factors should raise the clinician’s suspicion for an acquired UD.
Possible explanations for male UD include:
- Increased urethral pressure from a urethral obstruction, with consequent outpouching of the urethral epithelium. Particularly in patients with a background of reconstructive procedures for hypospadias, urethral stricture, trauma, or incontinence.15
- Following anorectal malformation repair from a retained portion of the urethral fistula ballooning out as more urine is sequestered in the herniated structure.16
- In patients with indwelling urethral catheters: the constant pressure at the penoscrotal angle with chronic urethral ischaemia, urethral fibrosis, and scar formation.17
The purpose of this paper is to present an updated review of acquired male UD according to clinical presentation, diagnostic imaging findings, management, complications, and outcomes.
MATERIAL AND METHODS
A literature search was conducted using Medline, Embase, and Cochrane databases in June 2015 to identify papers related to acquired male UD concerning type, aetiology, presentation, radiologic and/or surgical intervention, and outcomes. Publications not concerning humans were not considered. We identified original articles, review articles, and editorials addressing the subject. All articles published in the English language were selected for screening. The online electronic literature search involved unrestricted, fully explored Medical Subject Headings using terms related to secondary UD in adult men. Two independent reviewers selected all relevant articles and all duplicates were eliminated. The relevant articles were selected after reading the full text of the manuscripts and the eligibility criteria for inclusion was based on relevance concerning the subject. If there was any doubt concerning the eligibility of a study, abstracts and/or the full text were examined. Additional papers were identified from the reference lists of these articles.
CLINICAL PRESENTATION
Symptoms of UD vary dependent on the size, site, and degree of obstruction. Clinically, these patients may be completely asymptomatic. As expected, acquired UD patients present later than patients with congenital UD. The most common symptoms are obstructive lower urinary tract symptoms, postmicturition dribble, recurrent urinary tract infections, perineal pain, dysuria, urinary incontinence, with some cases of penile or perineal swelling, or even scrotal oedema.5,12 Haematuria is also a common finding and a full workup on its aetiology should be carried out.13
DIAGNOSIS
In a paper by Allen et al.,15 the most common location for both congenital and acquired diverticula is the penoscrotal angle, perhaps due to long-term urethral catheterisation. Large diverticulum can be diagnosed by palpation during clinical examination and the liquid content, if any, can be drained using this procedure (Figure 1).12 A diverticulum of smaller dimension requires specific imaging to be identified and to efficiently decide on adequate management.12

Figure 1: Enlarged urethral bulging mass corresponding to an anterior diverticulum.
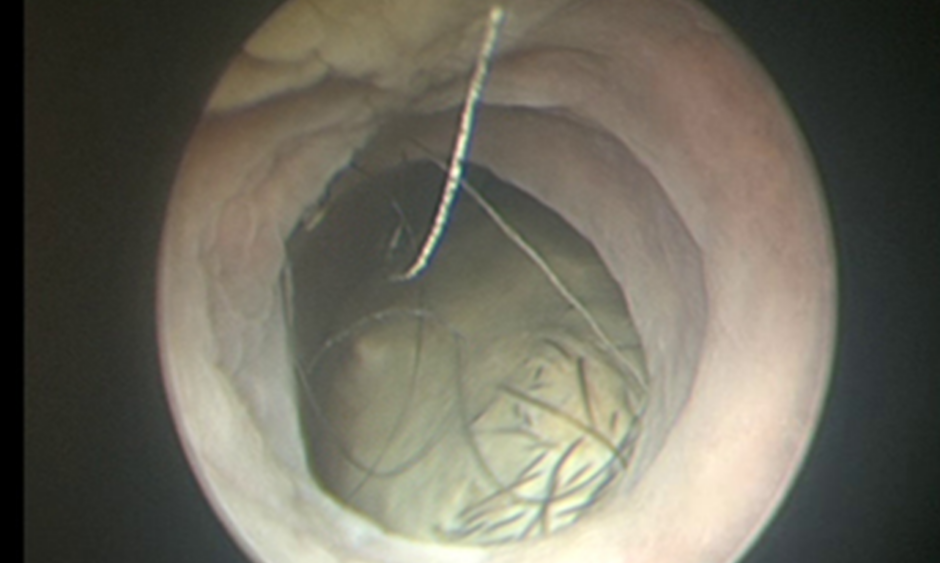
Conventional contrast studies, including ascending urethrography and voiding cystourethrography, along with urethrosonography and cystourethroscopy, are recommended for an adequate diagnosis of UD (Figure 2). Additional imaging may be required if a distorted anatomy is present and to delineate a surgical strategy.5,18

Figure 2: Urethral diverticulum with visible calculus on urethroscopy.
Using high-frequency linear probes and the intermittent introduction of normal saline solution to distend the urethra, the anterior urethra and perineal tract can be examined. The bulbar urethra should be scanned by placing the probe longitudinally on the ventral surface of the penis, or transperineally after having lifted the scrotum. Transversal scans can be used to explore focal lesions.1
Magnetic resonance imaging (MRI) is a sensitive and specific technique that has been proven effective at determining the size and extent of UD in women, but clinicians still lack experience when dealing with male urethra given the scarcity of these situations;19 additionally, it is a costly and not easily accessible procedure, which precludes its use as a first-line examination.20 Despite this, diagnosis and management of UD is greatly improved with this technique and cross-sectional imaging is increasingly being used in association with the former techniques; thus, this allows the clinician to clearly define the extent and location of the diverticulum, the integrity of the support structures, and to choose whether to perform an endoscopic or open surgical excision.13
MANAGEMENT AND OUTCOMES
Treatment should be individualised according to the location and size of the diverticulum, the presence of concomitant infection, and other pathologic findings that may need to be addressed. Small asymptomatic lesions may be monitored, particularly if the UD can be manually emptied. Some authors advocate a first-line approach with endoscopic incision of the diverticulum by transurethral unroofing if the integrity of the corpus spongiosum is intact and a good surrounding supportive tissue exists,10,13,21 which is evidenced by the lack of a bulge in the penis or scrotum during micturition. Despite being a technically easier option, the rate of UD recurrence and urethrocutaneous fistula is higher than in open procedures.3 Scar tissue formation and subsequent urethral stricture is also a possible outcome after endoscopic approach.13
An open procedure should be selected if an endoscopic approach is deemed to be unsuccessful, in the presence of recurrent urinary tract infections despite antibiotic therapy, or if there is an obstructive voiding or a stone in the UD (Figure 3).3 Open management options include primary anastomosis after UD excision or substitution urethroplasty, restoring urethral continuity while providing a good vascular network and an adequate support structure. A flap or two-stage repair may be an option, both of which are the most risk-free techniques.5 The risk of urethrocutaneous fistula with the possibility of additional surgical procedures (especially if a primary procedure was carried out) means that interposition of additional healthy tissue between the urethra and the diverticulum (e.g., dartos fascia) may be a good preventive measure.5,21
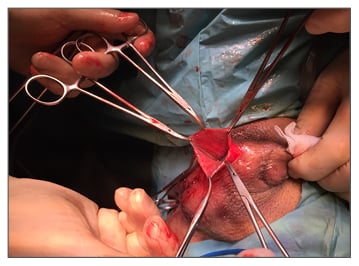
Figure 3: Open surgery for removal of a large anterior urethral diverticulum.
Cases of epididymo-orchitis following catheter removal have been reported.3 Consequently, it is recommended that urethrography and prophylactic oral antibiotics are administered postoperatively until catheter removal in order to confirm success of the procedure.2 If a patient is unsuitable for surgery (e.g., multiple urethral surgeries, extensive fibrosis from local radiation, or anatomical abnormalities) urinary diversion can be a suitable option.3 It may also be appropriate in patients with neurogenic bladders for whom frequent urethral catheterisation is to be expected, compromising urethral healing or even increasing the risk of UD recurrence.3
In a paper from Parker et al.,22 <100 cases of urethral carcinoma resulting from UD were reported. It occurs more often in women than in men, with a typical squamous or clear cell adenocarcinoma differentiation. Given this fact, freezing sections of the diverticular walls during its resection may be advisable.
CONCLUSION
A male acquired UD is a rare finding. It must be considered in the differential diagnosis of suspicious penile and scrotal masses, and if a large diverticulum is found. If there is significant urinary stasis, recurrent urinary tract infections, or urethral calculi, a rigorous and thorough clinical examination followed by surgical correction is most often standard procedure, allowing for treatment of symptoms and aetiology simultaneously. Reconstructive urethral surgical corrections are very complex, requiring a specialised approach, and are often found only in high-volume surgical centres. Other patients may be managed with urinary diversion only, rather than surgery.