INTRODUCTION AND OBJECTIVES
In addition to the evaluation of voiding symptoms, the medical evaluation (history and diagnostic tests) of patients with nocturia should also consider other related causes, such as sleep disorders, obstructive sleep apnoea (OSA), diabetes, and heart failure. The overall objective of this survey was to study the discrepancy between the recommendations made in the European Association of Urology (EAU) guidelines on the evaluation of nocturia and the clinical practice of Dutch urologists and urology residents.
MATERIALS AND METHODS
A national cross-sectional survey was sent digitally to 450 urologists and urology residents in the Netherlands. The questions were related to their work setting, field of interest, the number of patients with nocturia, the questions they ask when recording patient history, and the diagnostic adjuncts applied in the evaluation of patients with nocturia.
RESULTS
A total of 113 questionnaires were eligible for analysis. The distribution of the work setting and field of expertise of the urologists is shown in Figure 1. During history taking, almost all the urologists reported asking patients with nocturia about their storage (93%) and voiding complaints (83%), voiding frequency (98%), fluid intake (89%), and symptoms suggestive of heart failure (82%). However, questions about sleep disturbances (47%) and alcohol consumption (47%) were asked by less than half of the urologists and residents when evaluating nocturia patients. Questions about symptoms suggestive of diabetes (38%) or OSA (36%) were only asked by around one-third of the urologists in this survey. The results of the questions asked during patient history and additional diagnostic test are summarised in Figure 2.
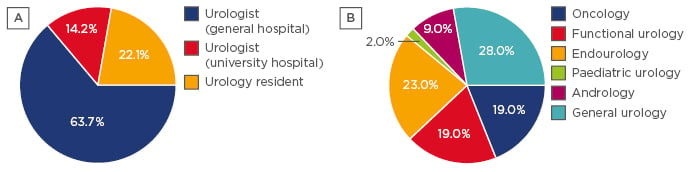
Figure 1: The distribution of Dutch urologists surveyed on the basis of their work setting (A) and their field of interest (B).
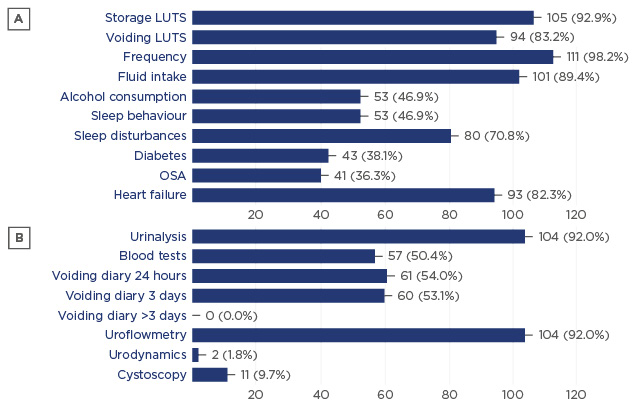
Figure 2: Results of a survey sent to Dutch urologists. The figure shows the percentage of urologists who asked questions about specific topics during patient history (A) and who reported use of diagnostic tests (B).
LUTS: lower urinary tract symptoms; OSA: obstructive sleep apnoea.
DISCUSSION AND CONCLUSIONS
Although most European urologists claim to apply the EAU guidelines, adherence to them is low in daily practice. This survey shows that only a minority of the Dutch urologists and residents ask about alcohol consumption and symptoms suggestive for diabetes or OSA.
In addition, most of the doctors reported using a bladder diary for either 24 hours or up to 3 days, despite the EAU guidelines grade of recommendation A and level of evidence 2b on the use of a bladder diary for the duration of at least 3 days and up to 7 days.1
Regarding the evaluation of patients with nocturia, the results from this study allow the conclusion that the use of a voiding diary for a sufficient length of time (a minimum of 3 days), as well as questions regarding OSA, diabetes, and alcohol consumption, are not applied by the majority of urologists in the Netherlands, which could reflect the clinical practice in other European countries. This observation mandates better education and campaigns to raise awareness on these matters.








