Prostate biopsy is currently an essential procedure for prostate cancer diagnosis and the transrectal approach is most commonly used by European urologists.1 Even though transrectal prostate biopsy (TR-PB) is generally considered a safe procedure, it may be accompanied by several clinical complications.2 In the last few years, we have observed a higher number of infectious complications reported after the procedure compared with other complication types.1-3 The higher rate of sepsis could be due to the emerging resistance to fluoroquinolones.3-4 Today, the infective complications after TR-PB represent an important challenge for the urologist and a life-threatening risk for the patient, in particular due to the increased rate of antibiotic-resistant bacteria. We need to focus our attention on the prevention of infective complications and find novel approaches and strategies.
INFECTIVE COMPLICATIONS: THE SIZE OF THE PROBLEM
Even with fluoroquinolones being the most prescribed drug for TR-PB prophylaxis, in line with European Association of Urology (EAU) guidelines,5 the hospital admission rates due to complications following TR-PB have increased dramatically during the last 10 years.3,6 The recently published results of the Global Prevalence Study of Infections in Urology study showed a high rate of symptomatic urinary tract infections (5.2%) and a significant rate of hospitalisation (3.1%).3 In the same study, Wagenlehner et al.3 reported that fluoroquinolones were administered to 98.2% of patients, in accordance with the EAU guidelines, but the resistance rate against fluoroquinolones was seen in 60% of all isolated bacterial strains. Moreover, several studies showed that the higher risk of infection is due to an increase in ciprofloxacin resistance in Escherichia coli and hence a concomitant decrease in the efficacy of ciprofloxacin prophylaxis in patients undergoing TR-PB.7 The recent increase of fluoroquinolone- resistant organisms has become a true contemporary health emergency (Figure 1). This condition is due both to the misuse and over-prescription of antibiotics and the limited research on new molecules, meaning that there is a reduced number of new antibiotics planned by pharmaceutical companies.6
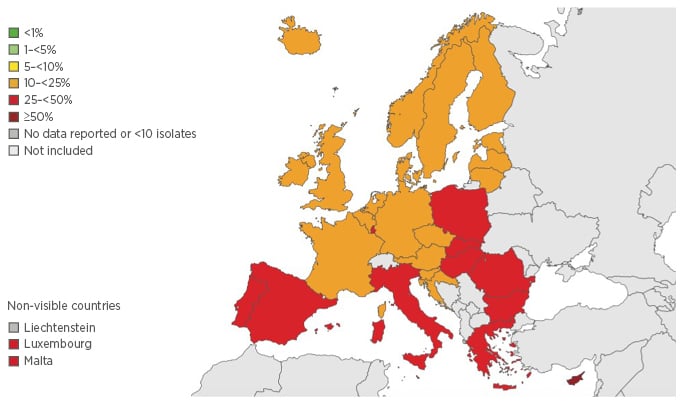
Figure 1 Percentage (%) of invasive isolates with resistance to fluoroquinolones, by country, EUEEA countries, 2013. Antimicrobial resistance surveillance in Europe, 2013. Annual report of the European Antimicrobial Resistance Surveillance Network.10
INFECTIVE COMPLICATIONS: ALTERNATIVE STRATEGIES TO DECREASE INFECTIVE COMPLICATIONS
Several strategies have been proposed and evaluated to prevent infective complications after TR-PB:
- Risk assessment to select patients at higher risk for infective complications:
Identify patients at higher risk of infective complications - Microbiological sampling of the faecal flora prior to biopsy to identify resistance to specific agents:
Consider that rectal swab would represent a substantial burden for clinical microbiology laboratories and might fail to detect ciprofloxacin-sensitive isolates with borderline minimum inhibitory concentrations - Biopsy cores and the use of targeted, image fusion guided biopsies and change of biopsy route (perineal approach):
Even if TR-PB is convenient, cheap, and quick to perform, please consider the transperineal approach as an option to all patients in whom a high risk of infective complication has been found - Alternative antibiotics with improved susceptibility to be used for prophylaxis:
The rising resistance to fluoroquinolones such as ciprofloxacin is the most likely cause of the increasing prevalence of infectious complications after TR-PB, and novel approaches for antibacterial prophylaxis need to be designed and evaluated accordingly. Fosfomycin seems a candidate alternative agent for antibiotic prophylaxis in TR-PB, having shown elevated activity against multidrug-resistant Gram-negative bacteria and favourable pharmacokinetic parameters, including an elevated penetration into prostatic tissue8-9
TAKE HOME MESSAGES
In conclusion, from all the evidence it is clear that prostate biopsy policy should be totally revised in order to obtain acceptable prospective results in terms of infective complications, cost saving, and patient compliance. In everyday clinical practice, please take into account the following aspects:
- A detailed evaluation of all risk factors for infectious complications (i.e. diabetes and previous use of antibiotics for urinary tract infections)
- Evaluation of all risk factors for harbouring resistant organisms (i.e. recent hospitalisation, travel to certain geographical regions, or antibiotic use)
- The role of alternative strategies for reducing the risk of infective complications








