Bladder cancer represents one of the most common malignancies diagnosed in both males and females, with an estimated 79,030 new cases and 16,870 estimated deaths in the USA in 2017.1 It is important to monitor bladder cancer patients, given the high risk of both recurrence and progression, through regular endoscopic surveillance with cystoscopy following the first transurethral resection of the bladder tumour (TURBT).2 Although conventional white light imaging (WLI) cystoscopy and TURBT are the standard methods for detecting urothelial tumours,2 the use of WLI could lead to approximately 10–20% of lesions that are not readily visible being overlooked.3 As a result, novel technologies are being developed in order to improve the detection rate and allow a more accurate diagnosis that can positively impact patient prognosis.
Blue light cystoscopy, also known as photodynamic diagnosis (PDD) fluorescence cystoscopy, was first described in 19644 and has gained popularity over the years.5 Narrow band imaging (NBI) is another valid technique, which works by filtering the white light into specific light wavelengths that are absorbed by haemoglobin, and only penetrate the surface of human tissue, enhancing the visualisation of mucosal vasculature and highlighting neoplastic neoangiogenesis of urothelial tumours.2 The aim of the present study was to accomplish a comprehensive systematic review and diagnostic meta-analysis to compare oncological outcomes, as well as evaluate the diagnostic accuracy of WLI, NBI, and PDD for detecting overall bladder cancer at an individual biopsy level. Eligible studies were divided into three categories: first, randomised clinical trials comparing 5-aminolevulinic acid versus WLI; second, randomised clinical trials comparing hexaminolevlinate versus WLI; and third, randomised clinical trials comparing NBI versus WLI. No trials were excluded. The study is registered with PROSPERO, number CRD42017069333.
The systematic literature search initially yielded 1,606 articles. After removing 532 duplicates, the screening of the remaining 1,074 titles and abstracts generated 326 potentially eligible original articles. The pooled data showed a sensitivity of 0.93 (95% confidence interval [CI]: 0.76–0.98), 0.97 (95% CI: 0.91–0.99), and 0.80 (95% CI: 0.65–0.90) for PDD, NBI, and WLI, respectively, and a pooled specificity of 0.31 (95% CI: 0.10–0.63), 0.64 (95% CI: 0.48–0.78), and 0.57 (95% CI: 0.39–0.74) for PDD, NBI, and WLI, respectively. The heterogeneity of WLI was significant for specificity (Chi-square: p=0.00; I2: 98.59) and sensitivity (Chi-square: p=0.00; I2: 98.69); of NBI for specificity (Chi-square: p=0.00; I2: 87.20) and sensitivity (Chi-square: p=0.04; I2= 57.69); and of PDD for specificity (Chi-square: p=0.00; I2: 99.35) and sensitivity (Chi-square: p=0.00; I2= 99.70). The diagnostic odds ratios for PDD, NBI, and WLI were 6.18 (95% CI: 0.57–66.40), 54.11 (95% CI: 27.73–105.60), and 5.31 (95% CI: 1.74–16.22), respectively. The derived area under the curve from the hierarchical summary receiver operating characteristic showed an accuracy of 0.92 (95% CI: 0.89–0.94), 0.77 (95% CI: 0.73–0.81), and 0.75 (95% CI: 0.71–0.79) for NBI, PDD, and WLI, respectively (Figure 1).
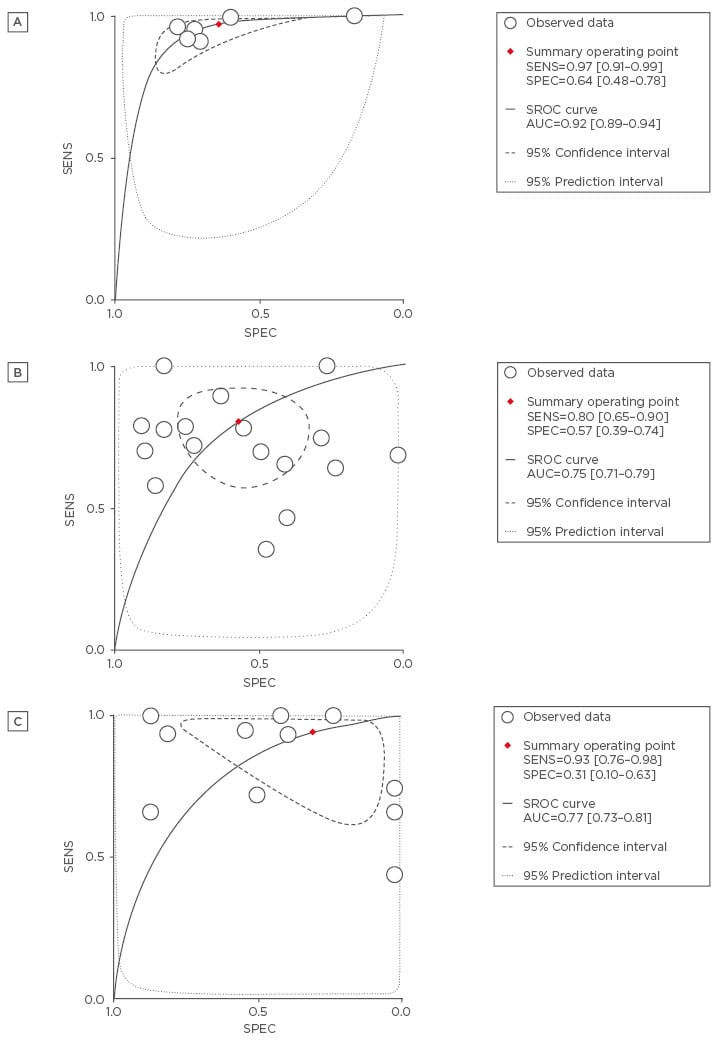
Figure 1: Hierarchical summary receiver operating characteristic plot (solid line) and summary point with 95% confidence interval (circled area) of A) narrow band imaging, B) white light imaging, and C) photodynamic diagnosis, in predicting overall bladder cancer.
Figure 1: Hierarchical summary receiver operating characteristic plot (solid line) and summary point with 95% confidence interval (circled area) of A) narrow band imaging, B) white light imaging, and C) photodynamic diagnosis, in predicting overall bladder cancer.
In this diagnostic meta-analysis, it was demonstrated that PDD and NBI exhibited lower recurrence rates and greater sensitivity than WLI. These results provide a step forward in abandoning WLI for the diagnosis and follow-up of bladder cancer. Despite this, patients who may benefit from WLI in terms of cost and efficacy must not be discriminated against, and PDD or NBI should replace standard cystoscopy.








