Introduction
Abdominal sacrocolpopexy is associated with a lower rate of recurrent vault prolapse, a reduced grade of residual prolapse, a longer time-to-recurrence, and less dyspareunia compared with the vaginal procedures such as sacrospinous ligament fixation and uterosacral ligament suspension. A recent Cochrane review stated that abdominal sacrocolpopexy is the more effective procedure and is considered by many authors to be the gold standard in the treatment of vaginal vault prolapse. Our objective is to evaluate the efficacy of laparoscopic sacrocervicopexy for apical support in sexually active patients with pelvicorgan prolapse.
Methods
Fifty women with symptomatic prolapse of the central compartment (Pelvic Organ Prolapse Quantitative [POP-Q] Stage 2) underwent laparoscopic sacrocervicopexy. We used Gynemesh PS™ Mesh, which is constructed of knitted filaments of polypropylene. It is a non-absorbable mesh, with excellent strength, durability, and porosity for necessary tissue in growth.
The operating physicians used the synthetic mesh to attach the anterior vaginal wall, posterior vaginal wall, elevator muscles in both sides, and uterosacral ligaments to the sacral promontory without hysterectomy. No anti-incontinence surgery was performed at the same time, even if the patient was incontinent. The patients returned for follow-up examinations 1 month after surgery and then over subsequent years. On follow-up a physician evaluated each patient for the recurrence of genital prolapse and the recurrence of de novo development of urinary or bowel symptoms. We define ‘surgical failure’ as any grade of recurrent prolapse of Stage II or more on the POP-Q test.
Patients also gave feedback about their satisfaction with the procedure using an analogue visual scale, graded from 0–10. Sexual activity was evaluated with the Index of Female Sexual Function (IFSF) questionnaire, which studies six items: desire, arousal, lubrication, orgasm, satisfaction, and pain (Table 1). Incontinence was also evaluated with the International Consultation on Incontinence Questionnaire (ICIQ-SF). This includes the following sections: S3: How often do you leak urine?; S4: Would you like to know how much urine you leak?; and S5: Overall how much does urine leakage interfere with your everyday life? (Table 2).
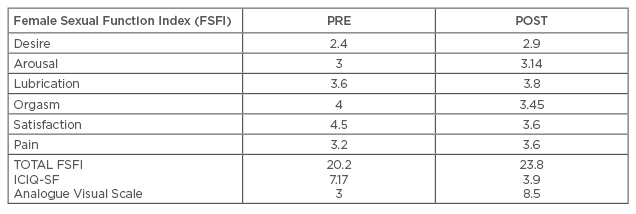
Table 1: Subjective results.
ICIQ-SF: International Consultation on Incontinence Questionnaire-Short Form.
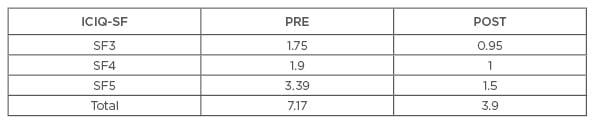
Table 2: International Consultation on Incontinence Questionnaire-Short Form (ICIQ-SF) questionnaire results.
Results
- The mean follow-up period was 33 months and the success rate was 90%
- The present study showed an 8.5/10 satisfaction rate
- A high amelioration on incontinence satisfaction, ICIQ-SF 8 versus 2.4 (range 0–21) was displayed. Twenty-two percent were incontinent before surgery
- Only 45% of patients required further incontinence surgery with a Miniarc®. Total incontinence surgery was 10%. The incontinence cure rate was 77.7%, incontinence maintenance was 11.1%, and de novo stress urinary incontinence was 2.86%
- Sexual results showed no changes (IFSF 22.75 versus 22.79, no SD)
- No changes in dyspareunia were shown
- Complications: 50% had bowel dysfunction, 5.7% mesh erosion, 2.8% bowel injury during the surgery, and 2.8% iliac injury.
- POP-Q results:
- Aa -1±1.8 versus -2±0.4
- Ba +1±2.3 versus -2±1.5
- C -1±3.4 versus -6±1.2
- Ap -2±1.3 versus -3±0.6
- Bp -2±3.1 versus -3±3.2
- Cystocele recurrence 6.8%
Conclusion
- Laparoscopic sacrocervicopexy is an effective option for sexually active women with pelvic organ prolapse
- No other incontinence surgery should be undertaken at the same time due to the risk of overtreatment








