BACKGROUND AND AIMS
Hospital-acquired infections represent a global healthcare crisis, contributing to patient morbidity and mortality.1 In response to the COVID-19 pandemic, hospitals had to re-organise wards, postpone elective procedures, and cancel non-urgent activities. Measures to limit the spread of the disease included restrictions to patients’ visitors, avoidance of street clothes by healthcare professionals, frequent object disinfection, and improved hand hygiene. Some of these measures have been shown to lower the rate of hospital-acquired infections and, as a result, the authors hypothesised that the occurrence of post-operative infection during the pandemic would be lower.2,3 The objective of the authors’ study was to compare the rate of post-operative infections and patterns of antimicrobial resistance before and during the pandemic in urology departments.
MATERIALS AND METHODS
This was an observational retrospective cohort study carried out in two Portuguese centres. Data from all elective surgical procedures between April and June 2018 and the homologous period in 2020 were collected.
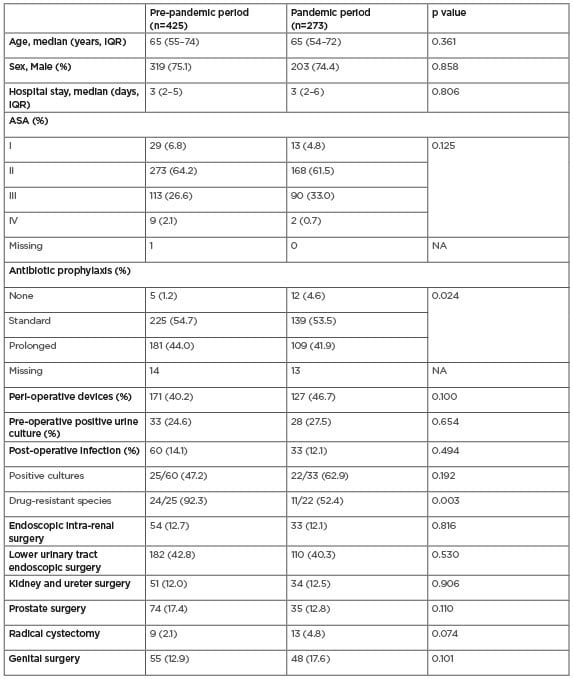
Table 1: Demographics and characteristics of patients submitted to elective urological surgery.
ASA: American Society of Anesthesiologists; IQR: interquartile range; NA: not applicable.
Patient data included age, sex, post-operative in-hospital length of stay, American Society of Anesthesiologist (ASA) score, type of procedure, antibiotic prophylaxis, pre-operative urine cultures, peri-operative use of medical devices, post-operative infections, microbial culture, and antimicrobial susceptibility testing. Infection was defined according to the European Centre for Disease Prevention and Control (ECDC) protocol. Multidrug resistant (MDR) organism was defined as a micro-organism resistant to one or more classes of antimicrobial agents tested. The main outcomes were the number of post-operative infections during the pandemic and the number of MDR isolates.
RESULTS
Baseline characteristics are presented in Table 1. The post-operative infection rate during the pre-pandemic period was 14.1% compared with 12.1% during the pandemic (p=0.494). Ninety two percent of isolates were MDR in the pre-pandemic period compared with 52% during the pandemic (p=0.002). The pandemic period was associated with a reduced risk for MDR isolates on multivariate logistic regression analysis (odds ratio: 0.1; 95% confidence interval: 0.07–0.57; p=0.010), but not with reduced number of infections (odds ratio: 0.84; 95% confidence interval: 0.53–1.34; p=0.47).
CONCLUSION
MDR isolates were lower during the pandemic in urology wards, possibly as an indirect result of COVID-19 preventive measures such as increased hand hygiene, room disinfection, and reduced family visits to inpatients. No statistically significant difference was found between the number of post-operative infections in the authors’ sample. Further reports such as those from the ECDC are needed to confirm the authors’ results.








