Robot-assisted laparoscopic prostatectomy (RALP) has become a standard treatment in the management of localised prostate cancer; however, erectile dysfunction (ED) and incontinence remain the major side effects of RALP, despite advances in surgical techniques. The incidence of postoperative ED ranges from 10–46% and the condition is the leading cause of patient dissatisfaction after RALP.1 Several surgical refinements have been described to enhance functional recovery, including athermal neurovascular bundle (NVB) dissection and minimal NVB traction during nerve-sparing (NS) RALP.1,2 Even in patients with good NS, there is a convalescence period due to surgical trauma-induced inflammation, neuropraxia, and nerve injury,2 which leads to delayed functional recovery.
The use of growth factors and anti-inflammatory substances is a novel concept for the prevention of the inflammatory response and neuropraxia in NVB. Dehydrated amnion/chorion membrane (dHACM) contains numerous growth factors and anti-inflammatory mediators that have proven clinical benefits in nerve healing.3,4 Our group was the first to propose enhanced NVB healing by application of dHACM in RALP patients. In our preliminary study of 58 patients, we found that NVB wrapping with dHACM accelerated continence and potency recovery at 8 weeks.5 The current study represents further testing of our hypothesis in a larger patient population with up to 18 months follow-up.
In this study, all consecutive men who received dHACM wrapping of the NVB during RALP between August 2013 and December 2016 were analysed (Group I [n=440]). The control group was selected by propensity score matching for age, Gleason score, D’Amico risk category, and preoperative sexual health inventory for men (SHIM) score (logistic regression nearest neighbourhood method at 1:1 ratio). Oncological and functional outcomes were compared between the two groups. Factors affecting potency recovery were analysed using univariate and multivariate logistic regression analyses.
When the study groups were compared, there was no significant difference in continence (0–1 pad/day) rates at a median follow-up of 18 months (97.7% versus 97.2%; p=0.66). As compared to the control group, potency rates at follow-up were significantly higher (76.1% versus 66.4%; p=0.001; Table 1) and potency recovery was significantly faster (4.1 versus 5.7 months; p=0.001) in the dHACM group irrespective of age, preoperative erectile function, and degree of NS. On multivariate analysis, age, preoperative potency, NS status, and dHACM nerve wrapping were found to be independent predictors of potency recovery.
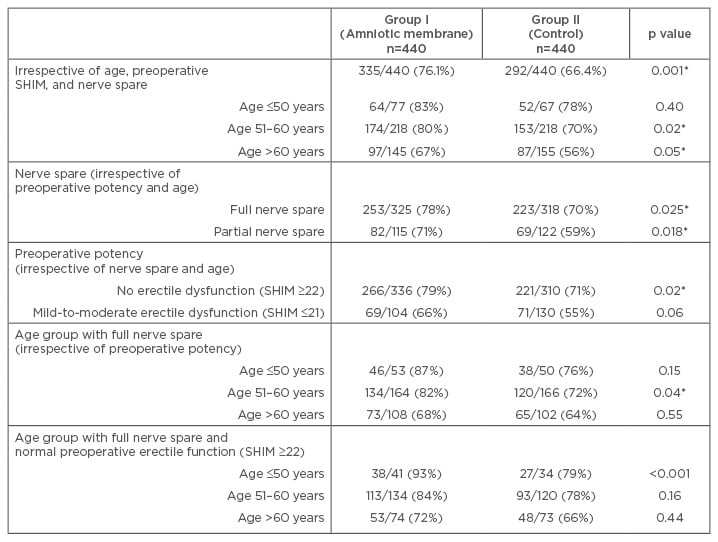
Table 1: Number of men who achieved potency after robot-assisted laparoscopic prostatectomy analysis based on age categories and preoperative erectile function.
SHIM: sexual health inventory for men.
*statistically significant.
The subgroup analysis showed that preoperatively potent (SHIM score ≥22) patients <50 years of age with complete NS benefited most from dHACM (postoperative potency of 93% versus 79%; p<0.001; Table 1). Furthermore, dHACM increased the potency rates whether a full bilateral or a partial NS was performed; this implied that dHACM graft can exert its healing effect on all branches of the NVB that can be preserved. Therefore, dHACM may serve as a valuable tool to optimise NS outcomes in high-risk prostate cancer patients whenever partial NVB preservation is more feasible than full NS due to concerns with increased surgical margin positivity risk. Future randomised studies will better clarify the clinical benefits of dHACM in functional outcomes after RALP.








