INTRODUCTION
Non-muscle invasive bladder cancer (NMIBC) can be treated by organ-sparing transurethral resection of bladder tumour (TURBT) but has a high risk of recurrence and probability of grade and stage progression. If recurrence is diagnosed at a very early stage, it can be treated in the outpatient clinic.1 As a standard, white light (WL) flexible cystoscopies are used in the surveillance programme. Photodynamic diagnosis (PDD) is an optical technique that uses fluorescence as a contrast mechanism to indicate pathologic tissue. Studies on PDD-guided TURBT have shown that up to 15% of non-invasive tumours and approximately 30% of flat carcinoma in situ may be overlooked by conventional WL cystoscopy.2 This randomised study aimed to investigate whether the use of PDD could reduce the number of recurrences when performing a follow-up flexible cystoscopy in the outpatient clinic. This abstract, presented at the 2018 European Association of Urology (EAU) Congress, presents the initial results of the treatment at the time of enrolment and randomisation.
MATERIALS AND METHODS
From February 2016–September 2017, 605 patients from three urological departments in Denmark were studied. All patients followed the Danish surveillance programme for NMIBC. Patients were randomised 1:1 to either an intervention group where hexaminolevulinate (Hexvix®; Photocure, Oslo, Norway) was instilled in the bladder 1 hour before the cystoscopy with PDD video cystoscope (PDD 11272 VPI, D-Light C-Light Source; Karl Storz, Tuttlingen, Germany), or a control group where cystoscopy was performed with a WL flexible cystoscope. In both patient groups, solitary or small (<1 cm) multiple recurrences, as well as suspect mucosa, were biopsied or fulgurated directly in the flexible procedure if possible or scheduled for a new TURBT.
RESULTS
A total of 304 patients were allocated to the intervention group (flexible PDD) and 301 to the control group (flexible WL). Approximately half of all patients in both groups were recurrence free (intervention group, n=157, and control group, n=150). The number of patients treated in the outpatient clinic was higher in the intervention compared to the control group. Thus, significantly fewer patients were scheduled for a TURBT in the intervention group (Table 1).
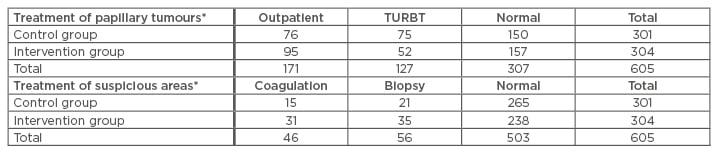
Table 1: Number of patients receiving treatment at time of enrolment and randomisation.
In the control group, cystoscopy was performed with a white light flexible cystoscope. In the intervention group, hexaminolevulinate was was instilled in the bladder 1 hour before the cystoscopy with a photodynamic diagnosis video cystoscope.
*p value: <0.05
TURBT: transurethral resection of bladder tumour.
CONCLUSION
These initial results indicate that PDD-guided flexible cystoscopy can reduce the need for TURBT when biopsy and fulguration of small tumours is possible in the outpatient clinic. Further follow-up data on long-term recurrence will be needed to estimate the clinical impact regarding the reduction of recurrence risk and repeated procedures.








