Erratum: Perspectives of the Methofill® (Methotrexate) Pre-filled Injector Device: Insights from a Rheumatology Nurse Consultant and Results from a Real Life Patient Experience Survey
Interviewee: Kate Hunt
Original citation: EMJ. 2021;6[3]:33-39.
Date correction published: 22.09.21
The interview with Hunt in EMJ 6.3 (pages 33-39) was originally published on 21.09.2021. Since then, an erratum has been made. On page 37, “Of those who expressed a preference in the survey11 47% (20/43) of patients” originally read “Of those who expressed a preference in the survey11 54% (20/37) of patients” incorrectly. This has now been updated.
The EMJ apologises for the error and any inconvenience caused.
Interviewee: Kate Hunt
Kingston Hospital NHS Foundation Trust, Galsworthy Road, Kingston upon Thames, Surrey, UK
Disclosure: Hunt has received sponsorship from UCB to attend the British Society for Rheumatology (BSR) meeting in April 2021 and has received an honorarium fee from Accord-UK Ltd with regard to this article.
Acknowledgements: Medical writing assistance was provided by Dr Brigitte Scott, MarYas Editorial Services, Cowlinge, UK.
Disclaimer: The views and opinions of the author are not necessarily those of Accord-UK Ltd, or of EMG, its publisher, advisers, or advertisers. No part of this publication may be reproduced in any form. Hunt was not involved in the survey.
Support: This article has been commissioned and funded by Accord-UK Ltd and developed in partnership with EMG-Health. Accord-UK Ltd suggested the topic and author and carried out full medical approval on all materials to ensure compliance with regulations. The sponsorship fee included honoraria for the author.
Citation: EMJ. 2021;6[3]:33-39.
INTRODUCTION
Rheumatoid arthritis (RA) is a chronic, progressive, inflammatory joint disease characterised by symmetrical inflammation of the peripheral joints and associated with cartilage and bone damage and substantial disability.1 This disease impacts significantly on occupational and daily activities, and is associated with increased mortality.2-5 RA is the most common autoimmune inflammatory arthritis, affecting approximately 1% of the population.6 A wide range of point and period prevalence of RA is reported in the literature, with average results of 51 in 10,000 and 56 in 10,000, respectively.7
Methotrexate (MTX) is one of the mainstays of treatment for active RA.8,9 MTX administered as a subcutaneous injection may overcome the limitations of oral MTX.9 However, needle phobia, patient treatment misconceptions, incorrect drug administration, and dexterity problems can reduce patient adherence to subcutaneous drug treatments.10
For this article, the EMJ conducted an interview on 12th May 2021 with Nurse Consultant Kate Hunt from Surrey, England, who has a wealth of experience and expertise in managing patients with active RA, to gain her perspective on the impact of active RA on adult patients and the benefits and challenges of self-injection MTX treatments for these patients. The results of a survey11 conducted to gain insight into patients’ experiences and perceptions of self‑injection MTX treatment were also discussed.
METHOFILL® (METHOTREXATE) SELF-INJECT PATIENT SURVEY
This was a cross-sectional, self-reported survey conducted between April 2019 and May 2020 on behalf of Accord‑UK Ltd in partnership with Day Lewis Pharmacy to gather real-life experience from 63 adults with active RA, psoriasis vulgaris, psoriatic arthritis, or Crohn’s disease using the Methofill® pre-filled injector device (Methofill SelfDose).11 The survey questionnaire captured anonymous data on experience of self-injecting MTX and perceptions of Methofill SelfDose (ease of grip, ease of use, preference, confidence, and satisfaction).11
IMPACT OF RHEUMATOID ARTHRITIS ON THE PATIENT
Hunt explained that the most frustrating aspects of active RA for patients include a lack of symptom patterns, and variable pain intensity and joint location, meaning that every day is different. Consequently, active RA may have a significant impact on quality of life: patients may need to adapt their life according to their symptoms, daily activities could be affected, and life might have to be planned, rather than spontaneous.
Joint discomfort is a key characteristic of active RA, and patients rarely achieve complete remission, Hunt claimed. Another important factor in active RA is fatigue, which Hunt considered is mostly joint-pain related and is sub-optimally managed.
Hunt observed that the huge psychological impact of a chronic disease such as active RA is increasingly being recognised, although psychological support services are limited by cost. She referred to the online information and support available for patients with active RA (e.g., National Rheumatoid Arthritis Society [NRAS],12 Versus Arthritis,13 NHS [UK National Health Service]14) as a positive improvement in active RA management; however, the ideal situation would be to have psychologists working alongside RA nurses to provide optimum care.
PATIENTS’ CONCERNS ABOUT TREATMENT FOR RHEUMATOID ARTHRITIS
The main concern patients with active RA have about treatment, Hunt remarked, is that MTX is a cytotoxic drug, and they fear it will give them cancer. Patients also worry about adapting to taking long‑term treatment, potential side effects (including hepatic and renal effects and nausea) and monitoring (liver function tests).
Hunt outlined how a motivational, persuasive approach by healthcare professionals encourages patients to adhere to treatment and open up about their concerns. She described patients with active RA as proactive and receptive to new treatment options.
TREATMENT ADHERENCE IN ACTIVE PATIENTS WITH RHEUMATOID ARTHRITIS
Treatment adherence is not specifically measured in the adult patients with active RA in Hunt’s care, but she defined adherence as reasonable. Hunt indicated the reasons for non-adherence are complex and relate to fear of side effects, perception of benefit versus side effects, comorbidities, concomitant medications, and the patient’s core beliefs about long-term treatment.15
Hunt summarised how, in her experience, non-adherence leads to disease progression, joint pain, seizing up/reduced mobility, and decreased quality of life.16,17 Non-adherent patients are offered extra information and training on their current treatment or are given an alternative treatment. For example, patients non-adherent to oral MTX (e.g., because of nausea, lack of efficacy) can be prescribed subcutaneous MTX.18 Hunt described MTX as the ‘baseline drug’ on which she aims to keep as many patients as possible “the long-term safety data around MTX is favourable.”19-21
KEY PATIENT NEEDS IN RHEUMATOID ARTHRITIS TREATMENT
Hunt has considerable experience of self-injection devices in patients with active RA and listed the key patient needs as a device that is simple to use, includes education (e.g., injection guides,22 nurse demonstration of technique using a dummy device, videos, online information), has individual support during the first injection, and diary or calendar reminders for administering treatment. Uptake of self-injection devices in her experience is good, as the devices are “designed around the patient.” Hunt identified easy to hold and easy and simple to use as crucial device-related factors, with the selection of which “patient-orientated” device is given to patients often depending on availability and cost.
MAIN CHALLENGES AND CONCERNS PATIENTS HAVE WHEN SELF-INJECTING METHOTREXATE
Hunt disclosed how patients who are new to self-injecting MTX worry about handling needles, and whether they will be able to use the device on days when their hands are particularly painful; psychological effects and barriers to accepting long-term treatment are also common.
The needle is hidden within the device in most designs, which reduces patient stress surrounding needle handling. Hunt acknowledged that many patients find these devices easy to operate, even on days when their hands are exceptionally sore, as they are “designed so well,” and commented that as the treatment is effective, “bad days” with debilitating pain might be less common. She specified that patients find self-injection easy once the technique has been demonstrated to them. Psychological difficulties are addressed with motivational guidance, training, and support. A total of 81% (46/57) of patients in the survey11 currently self-injecting MTX stated that they had no concerns or fears about self-injecting MTX (data on file: UK-03028), which indicates patients are generally less apprehensive once they are familiar with their treatment.
BENEFITS OF SELF-INJECTING METHOTREXATE TREATMENTS
Hunt noted the possible benefits of self-injecting MTX treatments for adult patients with active RA as potentially higher dose administration (and potentially increased efficacy) and fewer gastrointestinal side effects (e.g., nausea) than oral treatment,23-25 and delay or avoidance of administration of biologics.
METHOFILL SELFDOSE INJECTION DEVICE IS EASY TO GRIP
Hunt described the Methofill SelfDose injection device as bulkier than other MTX injection devices; therefore, patients with age- and/or disease-related poorer hand grip can hold the device without having to squeeze tight. She pointed out that the large handle on the device enables patients to use the base of their hand rather than their thumb to administer the injection.22 Hunt stated this is important for patients with overlapping active RA and osteoarthritis, as the latter particularly affects the thumbs and could make thumb activation of the device difficult.
Hunt commented that her patients “were able to hold the device without much grip at all.” The survey11 results support this observation: 75% (43/57) of patients strongly agreed/agreed that Methofill SelfDose was easy to grip while injecting (Figure 1; data on file: UK-01931).
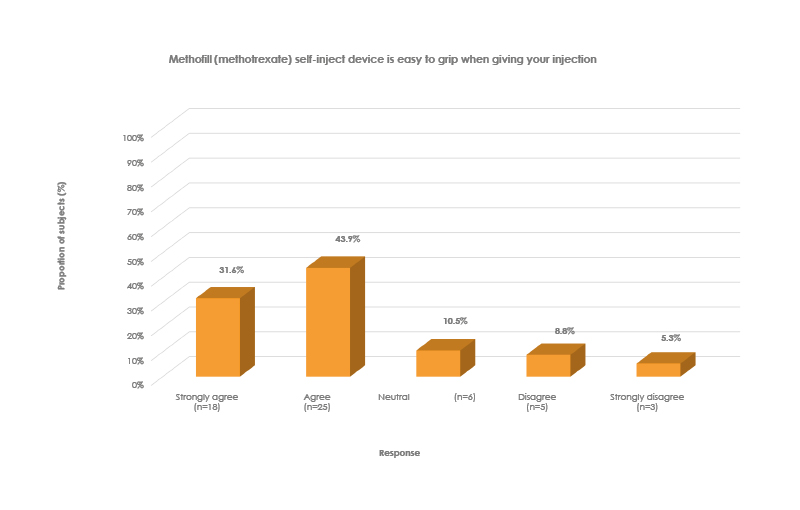
Figure 1: Patients’ view on ease of grip of the Methofill® self-inject device.
METHOFILL SELFDOSE INJECTION DEVICE IS EASY TO USE
Hunt is responsible for a large cohort of adult patients with active RA who use Methofill SelfDose, most of whom find it easy to use, have confidence in their device, and are treatment adherent (Hunt estimated that only approximately two of her >150 patients on Methofill SelfDose have switched back to their original device). In line with this, the survey11 showed that 75% (43/57) of patients strongly agreed/agreed that Methofill SelfDose was easy to use (Figure 2; data on file: UK-01943) and 89% (51/57) of patients strongly agreed/agreed that they were confident to inject Methofill SelfDose at home (Figure 3; data on file: UK-01944).
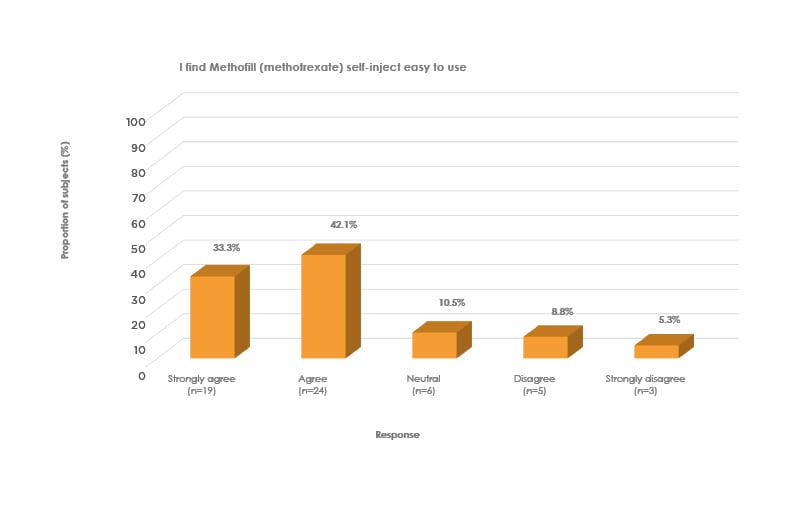
Figure 2: Patients’ view on ease of use of Methofill® self-inject device.
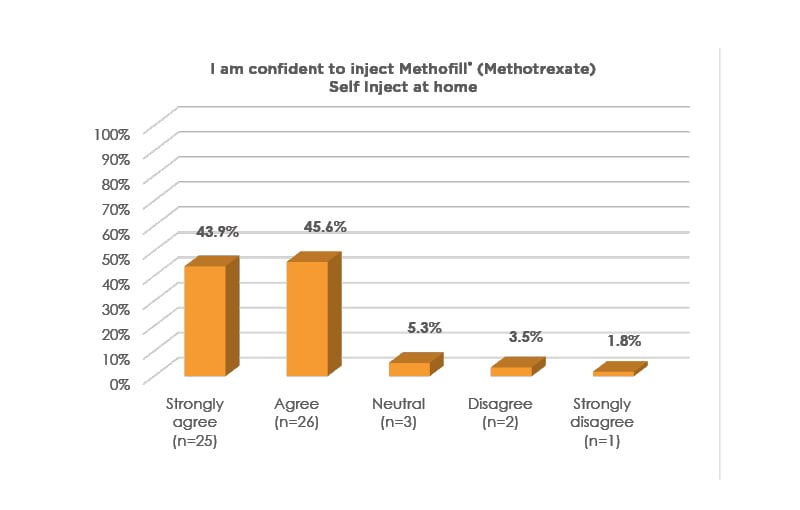
Figure 3: Confidence to inject Methofill® (Methotrexate) Self Inject at home.
PATIENTS ARE OPEN TO SWITCHING TO THE METHOFILL SELFDOSE INJECTION DEVICE
According to Hunt, patients with active RA are used to having their treatments changed and are amenable to switching devices provided they are informed beforehand and are reassured it is the same drug, just in a different device. Patients are supported through the switch to Methofill SelfDose with education and training.
Hunt clarified how patients who may not perceive a problem with their current self‑injection device are advised of the positive features of Methofill SelfDose, such as easy to grip, easy to use, and hand rather than thumb activation.
Of those who expressed a preference in the survey11 47% (20/43) of patients preferred Methofill SelfDose to their previous injection device (data on file: UK-01946). In Hunt’s experience, patients do not tend to express a preference for one device over another; however, good uptake of and adherence with Methofill SelfDose reflect acceptance of this device.
CONCLUSION
Hunt concluded that Methofill SelfDose benefits patients with active RA by helping to improve disease control and quality of life and is an effective way of giving the baseline drug, MTX, with ease and simplicity of use, enabling confidence in the device and good adherence. She reiterated that the design of Methofill SelfDose enables patients with poorer hand grip to hold the device without difficulty and administer the injection effectively with the base of their hands. In keeping with the 68% (41/60) of patients in the survey11 who were ‘satisfied’ (score of ≥7 on a scale of 1–10) with the Methofill SelfDose for administering their injections (data on file: UK-01945), Hunt judged the majority of patients in her care were satisfied with Methofill SelfDose.
Although there were limitations to the survey (small, anonymous patient cohort with unknown training and experience of Methofill SelfDose; no direct head‑to‑head comparison with other devices; no significant understanding of patient experience or perspective on previously used devices), the results concur with the insights from Hunt, indicating that Methofill SelfDose could be a positive tool to improve patient confidence, therapy adherence, and treatment outcomes in RA.
Biography
Nurse Consultant Kate Hunt
Kingston Hospital, NHS Foundation Trust
Hunt is currently a rheumatology nurse consultant at Kingston Hospital NHS Foundation Trust.
Hunt has been working in rheumatology for the over 25 years, having completed both a BSc in Health Studies at Surrey University, UK and an MSc in Rheumatology Nursing at Keele University, UK. She has been a non-medical prescriber for over 10 years.
Nurse Hunt’s role is very clinically based, focusing on managing patients’ long term conditions of inflammatory arthritis. Hunt also chairs the Hospital Nurses Specialist Group (NSG) and is an active member of the drugs and therapeutic group.
Uk-03046 Date of preparation: September 2021








