Key Points
1. Gout is a common rheumatological disease mimicking a wide variety of inflammatory conditions.2. Involvement of the hand is atypical requiring high index of suspicion to identify and investigate suspected patients.
3. Management should be tailored to individual patients by combining early surgical intervention with rheumatological assessment.
INTRODUCTION
Gouty arthritis, also called monosodium urate (MSU) crystal deposition disease, is an inflammatory disease where monosodium urate crystals build up in the joints and soft tissues, secondary to high uric acid levels in the blood.1 Due to its rarity, hand gouty arthritis is often excluded from the differential diagnosis. The authors report a unique instance of hand gouty arthritis manifesting as a soft tissue infection, which has been reported in line with the Surgical CAse REport (SCARE) 2023 criteria.2
CASE PRESENTATION
A 27-year-old male not previously known to have any medical illness presented to the emergency department complaining of right-hand soft tissue swelling and pain for 8 days. The swelling started in the right ring finger and extended proximally up to the elbow joint, associated with a limited range of motion. There was no history of hand trauma or a personal or family history of any rheumatological or autoimmune diseases. Ten days prior to his presentation, the patient underwent drainage of a right ring finger abscess. Upon examination, the right hand was oedematous with induration, hotness, and severe tenderness on palpation, with fluctuation over the middle and ring finger (Figure 1A).
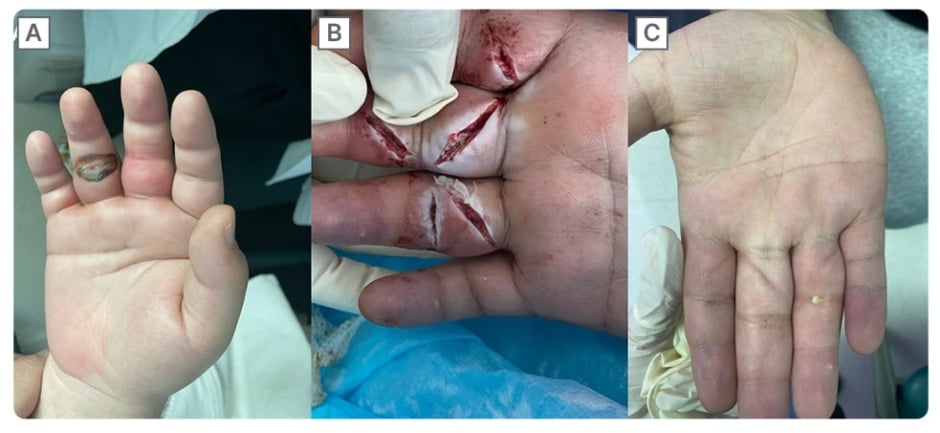
Figure 1: Pre- and post-operative pictures of the right hand.
(A) Preoperative picture of the right hand showing diffuse hand soft tissue swelling with erythema over the middle and ring finger.
(B) Z-shaped incisions over the right, middle, and ring fingers with thick whitish discharge.
(C) Post-operative picture with subsided swelling and erythema of the right hand and healed wounds.
There was a limited range of motion of the fingers, wrist, and elbow. His laboratory workup revealed a normal white blood count of 6.95×109. X-rays of the hand revealed soft tissue nodules on the middle and ring fingers. There were also lytic lesions on the second and third metacarpal bones and the proximal phalanx of the index finger (Figure 2).
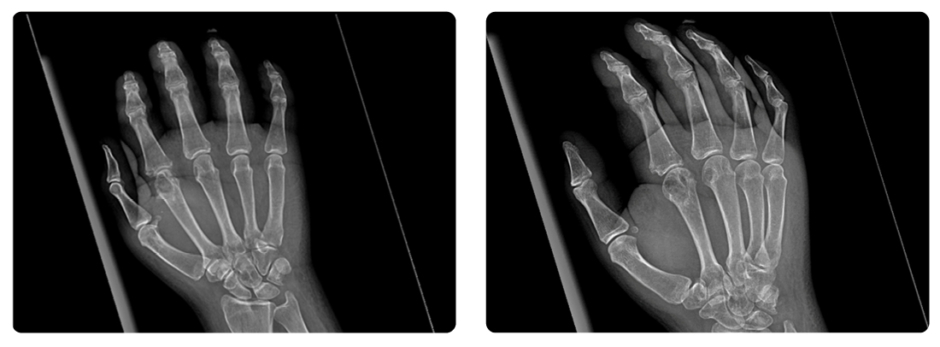
Figure 2: Hand radiograph showing soft tissue nodules over the middle and ring finger with lytic lesions on the 2nd and 3rd metacarpal bones and the proximal phalanx of the index finger.
The targeted hand ultrasound did not reveal any localised collection. The patient was admitted to the regular ward with the impression of hand cellulitis and a possible abscess collection. The patient started on intravenous antibiotics with no improvement. The patient was taken for an incision and drainage. During the operation, the surgeon made two Z-shaped incisions over the plantar aspect of the middle and ring fingers, along with a counter incision on the dorsal part of the middle finger. There was a thick, whitish material discharge from the wound that was sent for acid fast bacilli; cytology; bacterial, fungal, and mycobacterial cultures (Figure 1B). After the operation, the patient was kept on IV antibiotics and started hand exercises through physiotherapy. There was significant improvement in the oedema and pain, with slow improvement in his range of motion. An MRI scan of the right upper limb was used to determine if there was still a collection. The MRI showed synovitis in the metacarpophalangeal joint of the index, middle, ring, and little finger, but did not show any drainable collection during the scan. The results of all cultures and the cytology of the whitish discharge were negative for any growth. Subsequently, the patient was screened for rheumatological causes of inflammation. His serum urate measurement 5 weeks following the initial episode was 698 umol/L, and his erythrocyte sedimentation rate was 30 mm/hour. Gout was diagnosed based on his elevated serum urate, along with his clinical presentation. After discharge, the patient was followed in the outpatient clinic. He had significant improvement in his hand movement, and the wound healed with no remaining signs of inflammation (Figure 1C). He was able to resume his work with no limitation on his hand range of motion. The patient was referred to the rheumatology department for further management of gouty arthritis and initiating treatment with allopurinol and colchicine.
CLINICAL DISCUSSION
Gouty arthritis typically presents with pain, swelling, and erythema. It is sometimes associated with joint deformities in long-standing diseases. Doctors can easily recognise and diagnose it during an acute flare or in the presence of chronic tophi. Although gout commonly manifests as monoarticular disease, several cases have described patients presenting with polyarticular arthropathy. The first metatarsophalangeal joint is the most affected, especially during the first attack.3,4 Patients with no previous history of gout may not be aware of the unusual involvement of the hand in this condition, leading to potential missed diagnoses. These patients may present with entrapment neuropathy, tophaceous deposits infiltrating tendons, tenosynovitis or cellulitis, and abscesses, as seen in this case.4-6
There are three classifications of hand soft tissue infection: superficial, such as cellulitis; deep, such as abscess; and necrotising fasciitis. Swelling, erythema, hotness, and pain occur in patients due to the pressure within the confined space in the hand and digits. Untreated hand infections can progress to serious limb and life-threatening complications if not properly treated. Management involves antibiotics with drainage and debridement of any underlying collection and necrotic tissue.7 Previously, the literature reported the initial presentation of a gout-imitating hand abscess. The patient presented with acute and diffuse involvement of the hand, simulating an infection. During exploration, no pus was observed, and a negative fluid culture was obtained. Subsequently, the medical team investigated the patient and diagnosed them with gouty arthritis.6
Differentiation between gouty arthritis in the hand and soft tissue infection can be challenging, especially with an atypical presentation and multi-joint involvement as seen in this patient. Identifying urate crystals in the joint aspirate makes a definitive diagnosis of gout. However, this is not always clinically applicable, especially in the small joints of the hand, where patients may present without joint effusion to allow aspiration. High serum uric acid increases the risk of gout, but is not reliable in an acute attack of gout as it is often normal. The American College of Rheumatology/European League Against Rheumatism (ACR/EULAR) established the new gout classification criteria in 2015 to aid in the clinical diagnosis of gout (Table 1).3,4,8
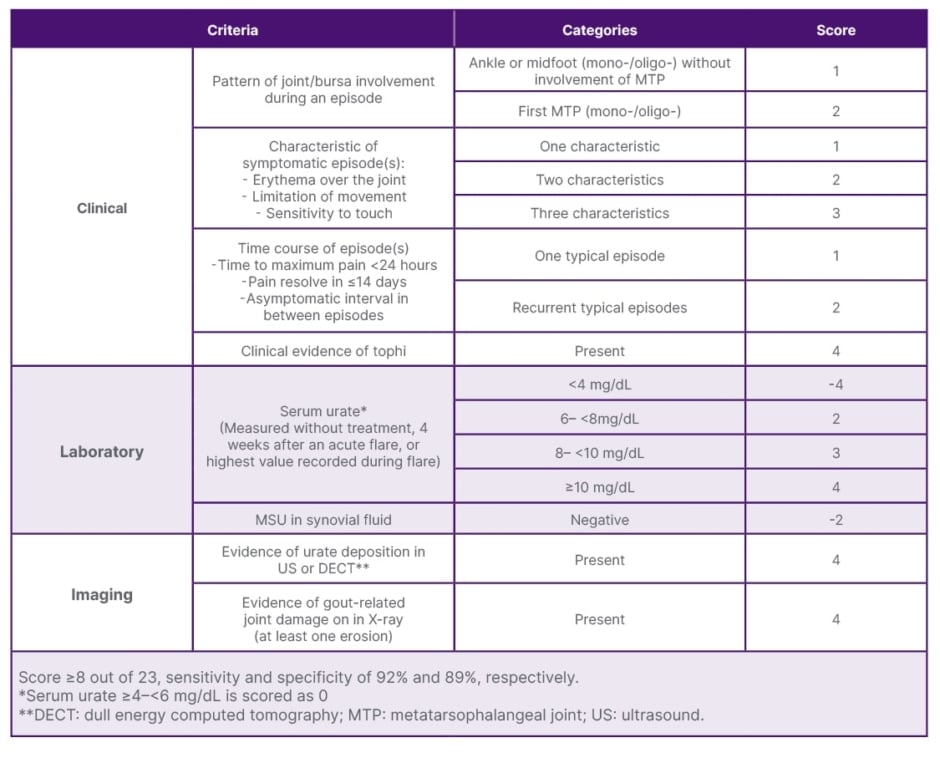
Table 1: The American College of Rheumatology/European League Against Rheumatism (ACR/EULAR) gout classification criteria.8
Both gouty arthritis and infections can cause non-specific elevations of inflammatory markers, such as erythrocyte sedimentation rate and C-reactive protein.4,9 The first line of treatment for acute gout flare-ups mostly involves non-steroidal anti-inflammatory drugs, colchicine, or oral corticosteroids. Long-term therapy with allopurinol and lifestyle modification aims to lower serum urate levels and prevent further crystal deposition.10,11 Certain patients undergo surgical interventions to achieve symptomatic relief of pain through nerve decompression and the evacuation of any underlying collection or source of infection. Excision of gout tophi is another indication for surgery in patients with a limited range of motion due to infiltration of the tendons by tophi.4,6,12
CONCLUSION
Gout is known to mimic a wide variety of inflammatory conditions, including soft tissue infections. Diagnosis of gout of the hand with such a presentation can be challenging. This case adds valuable insight into the diagnostic challenges and considerations when gout manifests atypically. The misdiagnosis of gout as a soft tissue infection highlights the need for clinical awareness and broad differential diagnosis in cases of hand swelling and pain, particularly when initial treatments fail. Current clinical guidelines for gout primarily focus on its typical presentations. Documenting rare cases like this case can stimulate further research into atypical presentations of common conditions and contribute to expanding the diagnostic guidelines to include rare presentations. This perspective can aid clinicians in avoiding diagnostic pitfalls and ensuring prompt and exact diagnosis, which is essential for optimal patient outcomes.







