BACKGROUND
Vasculitis is an umbrella term encompassing approximately 20 rare but serious diseases that are characterized by autoimmune inflammation and damage of the blood vessels. Patients living with vasculitis are considered immunocompromised and require further immunosuppression for the management of their autoimmune condition to prevent organ damage and death. Without immunosuppression, the mortality rate of some forms of vasculitis can reach 90% over 2 years. As a result of these two factors, there is an increased risk of vaccine-preventable diseases, which can result in increased morbidity and mortality in this patient population.1 Infection is, in effect, the leading cause of death in vasculitis.2-5 Due to this risk, vaccination is highly recommended for all patients with vasculitis6-7 but due to the rarity of this condition, a baseline rate of vaccination was not yet readily available. In this prospective quality improvement study, the authors’ aim is to provide Canada’s first baseline rate of vaccination in patients with vasculitis and implement a multidisciplinary strategy involving the patient’s rheumatologist and community pharmacists to improve vaccination rates.
METHODS
Hundred and three patients, between the ages of 18–89 (58% female), attending Calgary’s South Health Campus rheumatology clinic in 2023 were initially recruited to build a vaccination database. This database was created by reviewing papers and electronic charts. This determined the baseline vaccination status against pneumonia (PPSV23, PCV13, PCV20), shingles (RZV), tetanus (Tdap), hepatitis B, COVID-19, and influenza. Data pertinent to vasculitis subtype, treatment type, and demographics was also recorded. Patients were then contacted and provided with an overview and education of their missing vaccinations. All 103 patients who agreed to participate had their pharmacy of choice contacted by a member of the research team for their missing vaccinations. In-clinic reminders were also provided by intake nurses at the patient’s next visit. The vaccination status of patients in the database was reviewed at 1 year (2023–2024) to determine what improvements occurred in the overall vaccination rate. Patients with an incomplete/partial vaccine status were re-contacted to determine reasons for missing their vaccination(s) and were provided assistance in completing their vaccine series if they accepted (re-contacting the pharmacy, referral to public health, etc).
RESULTS
The baseline and final vaccination statistics of the 103 patients participating in VIVA QI can be seen in Table 1. The greatest vaccinated subgroup were those aged >65. The majority of participants self-identified as being White (79%), lived in a region with >100,000 people (80%), and had a primary care provider (89%).
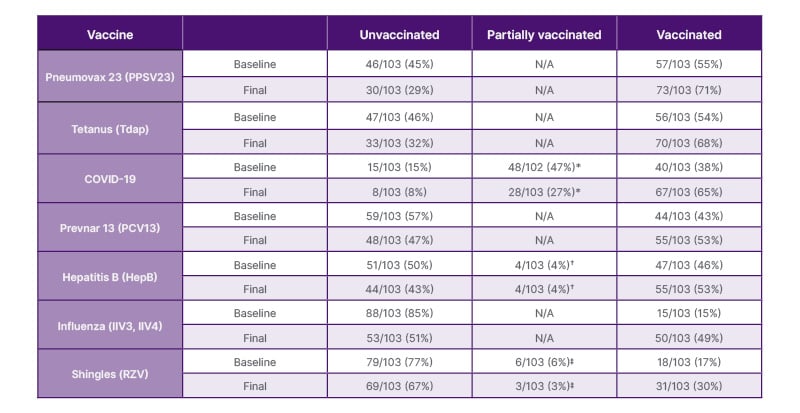
Table 1: VIVA-QI patient vaccination status at baseline versus after implementation of a multidisciplinary approach towards vaccination.
*COVID-19: receiving less than three mRNA vaccinations.
†Hepatitis B: receiving less than three vaccines.
‡Shingles: receiving one out of two vaccines in the series.
CONCLUSION
In this study, vaccination rates increased throughout all measured vaccines. The greatest improvement in vaccination rate occurred in vaccines which pharmacies could offer for free (influenza 34% increase, 233% year-over-year (YoY); COVID-19 26% increase, 68% YoY; PPSV23 16% increase, 59% YoY; and Tdap 14% increase, 25% YoY). Eighty-five percentage of the patients reported that the greatest barrier to vaccination was the cost of the vaccine. High degrees of trust were also expressed by patients regarding their healthcare providers; 91–96% of patients stated they trust their pharmacist, rheumatologist, and family physician’s opinion that vaccinations are safe. Due to VIVA QI’s multidisciplinary approach helping and educating patients, when compared to the provincial vaccination rates for the same time period, it resulted in greater vaccination rates (influenza 24.2% versus 49% and COVID-19 16.8 versus 46%, respectively). This study demonstrates the impact that a multidisciplinary approach has on a patient’s safety and care.







