There have been many studies about patient global assessments of disease activity in rheumatoid arthritis (RA) and how these differ from physician global assessments (MD global).1 The studies measure different things; when the rheumatologist is assessing patients with RA, disease activity is often based on swollen joints, their severity and distribution, and inflammatory markers, whereas patients may base their assessment on pain, damage, other musculoskeletal problems, and how they have been feeling recently, as opposed to disease activity. Physicians only see patients at a certain point in time, whereas patients may have flares and improvements of disease activity between visits; the latter would not be captured in the MD global if the flare had resolved.
The current study, presented at the European League Against Rheumatism (EULAR) 2018 Congress in Amsterdam, Netherlands, sent questionnaires to rheumatologists who are members of the Canadian Rheumatology Association (CRA) about patient scenarios of varying RA disease activity. They were asked to rate the disease activity on a scale of 0–10 for each case.2 Some cases involved follow-up visits so that the change in global assessment could be calculated. There was a response rate of approximately 30%.
The results showed that there was a wide variability of global assessments, but there was more agreement for extreme cases (low disease activity and high activity) (Figure 1). The cases in between these extremes had wide variability between physicians and little agreement. Agreement was in consensus for the change in global assessments for the scenarios that had follow-up visits, suggesting that rheumatologists may not agree on the score of disease activity but the change in activity was congruent (such as a lot worse, worse, same, better, or a lot better) as measured by a change in the global assessments. Rheumatologists who ranked themselves as experts in RA gave higher disease activity scores, which could mean that they did not tolerate disease activity and ranked any activity higher. The authors predicted that the scores of RA experts would be lower than their less experienced colleagues as they have seen so many cases and would be able to better contextualise a 10/10 score.
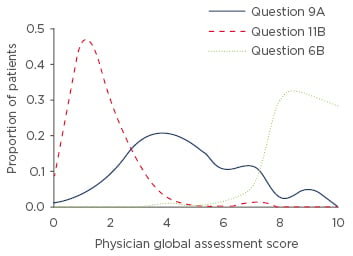
Figure 1: Global assessments of rheumatoid arthritis cases.
Cases that are extreme have more agreement than medium cases, as illustrated by the distribution of responses from these three scenarios.
This study is limited by focussing on cases on paper, rather than assessing real patients. The authors also had discordant patient global assessments wherein, for instance, a patient could be seen with no disease activity but ranked their pain and activity as 4/10, because this reflects real-world patients. In clinical practice, treating to a target includes low disease activity or remission as a goal so MD global should ideally be more standardised. This reflects what happens in the real world, and so there could be training for rheumatologists with a catalogue of scenarios to reach a better consensus (such as with a Delphi exercise) and it may mean that training for RA clinical trials is important since some scores have MD global in them (clinical [CDAI] and simple disease activity indices [SDAI])3 and remission rates can be very different depending on global assessments.








