The synovium is the primary site of the rheumatoid arthritis (RA)-related inflammatory process. One of the most noticeable signs of synovitis is the amount of synovial vascularisation, which is critical for synovial proliferation and invasiveness.1 Previous studies have showed the considerable ability of highly sensitive power Doppler ultrasound (PDUS) to improve the scoring of synovitis by detecting extended synovial vasculature.2 Only scarce data are currently available regarding correlations between systemic angiogenic activity, measured by angiogenic factors in the serum, and the amount of local synovial vascularisation, measured by Doppler ultrasound.3 The objective of this study was to investigate associations between synovial vascularity assessed by PDUS and a panel of eight serum vascular markers reflecting different angiogenic processes, such as endothelial cell activation, proliferation, survival, growth, and migration, as well as vessel maturation and stabilisation.
Serum levels of eight angiogenic markers (vascular endothelial growth factor, placenta growth factor [PlGF], Tie-2, angiopoietin-1, soluble vascular cell adhesion molecule-1 [sVCAM-1], IL-8 [CXCL8], CYR61 [CCN1], and angiostatin) were measured by quantitative ELISA in a total of 125 RA patients. The study participants were all systematically assessed in parallel by PDUS, performed on 32 joints. A global synovitis score, derived from the Global OMERACT-EULAR Synovitis Score (GOESS), was calculated for the 16 paired joints using the sum of the composite PDUS scores for all joints examined, giving a potential score of 0–96.
Synovitis was detected in 84 patients with RA (67.2%). Among these patients, 53 patients (42.4%) had a positive Doppler signal, including 31 with moderate-to-marked hyperaemia. Serum levels of sVCAM-1 (808±293 ng/mL versus 697±240 ng/mL; p=0.022) and Tie-2 (16.2±7.5 ng/mL versus 13.8±4.9 ng/mL; p=0.038) were more likely to be increased in patients with synovial hyperaemia detected on at least one joint (power Doppler Grade ≥1). sVCAM-1, Tie-2, and angiostatin concentrations gradually increased together with the grade of the semiquantitative PDUS scale, and concentrations of these three markers were markedly increased in patients with moderate-to-marked hyperaemia (power Doppler Grades 2 and 3) (Figure 1). Levels of sVCAM-1 (r=0.20; p=0.028), Tie-2 (r=0.28; p=0.001), and angiostatin (r=0.25; p=0.006) correlated with a global arthritis sum score, defined by the sum of the semiquantitative PDUS scores for all joints examined.
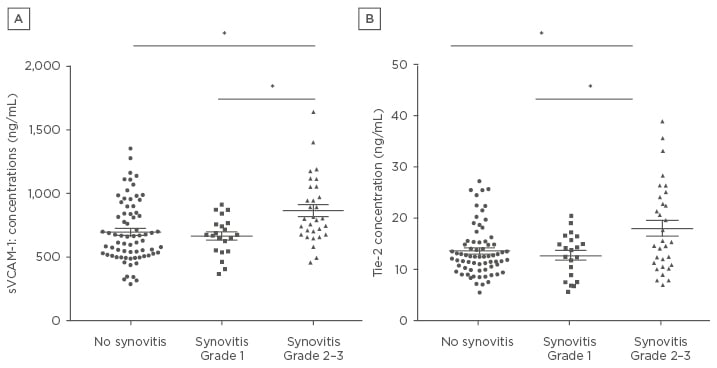
Figure 1: Levels of soluble vascular cell adhesion molecule-1 (A) and Tie-2 (B) according to the intensity and extent of synovial vascularisation assessed by power Doppler ultrasound.
Statistical analysis involved an analysis of variance (ANOVA) test followed by Tukey’s multiple comparisons test.
*p<0.01
sVCAM-1: soluble vascular cell adhesion molecule-1.
Among the 81 patients with a Disease Activity Score 28-joint count C-reactive protein ≤3.2, 22 patients had synovial hyperaemia detected on at least one joint (power Doppler Grade 1 in 13 patients, Grade 2 in 6 patients, and Grade 3 in 3 patients). Patients with synovial hyperaemia on at least one joint were more likely to have significantly increased levels of PlGF (18.9±11.2 pg/mL versus 13.1±9.5 pg/mL; p=0.022) and Tie-2 (15.7±5.8 ng/mL versus 12.6±3.4 ng/mL; p=0.004) than patients without synovial hyperaemia.
In conclusion, serum levels of the angiogenic markers Tie-2, sVCAM-1, and angiostatin were strongly associated with synovial vascularisation and inflammation assessed by PDUS among patients with established RA. Moreover, Tie-2 and PlGF were associated with persistent disease activity. These data highlight the possibility of identifying surrogate serum angiogenic markers of active synovitis and the need to confirm their pertinence in longitudinal studies.








