BACKGROUND AND AIMS
Interstitial lung disease (ILD) is a common pulmonary manifestation of rheumatoid arthritis (RA). It has emerged in recent studies as a key prognostic factor and affects rate of survival. The big challenge for rheumatologists is now the risk-stratification of patients with RA for ILD. Chest high-resolution CT (HRCT) is the gold standard for RA-ILD diagnosis, but costs and ionising radiation may limit its use in clinical practice. Thus, circulating biomarkers could aid in this risk-stratification. The authors’ objective was to evaluate the merit of three circulating markers for the diagnosis and the progression of RA-ILD.
MATERIALS AND METHODS
The study included consecutive patients with RA, >18 years of age, from three tertiary rheumatology centres (Paris, France; Tokyo, Japan; and Zurich, Switzerland) over a 36-month period. All patients had at least one chest HRCT during the inclusion period. In the subset of French patients with ILD, HRCT lung images were obtained both at baseline (time of blood sample collection) and at a follow-up visit. The ILD status of patients with RA was established by chest HRCT. The chest HRCT pattern was classified as usual interstitial pneumonia (UIP) or nonspecific interstitial pneumonia (NSIP) by the local radiologist. Serum levels of lung epithelial-derived surfactant protein-D (SP-D), C-C motif chemokine ligand-18 (CCL-18), and Krebs von den Lungen-6 glycoprotein (KL-6) were measured by ELISA.
RESULTS
In the study, 147 patients were included (age: 66±12 years old; females: 69%; males: 31%; disease duration: 11±10 years). Amongst these patients, 40 (27%) had fibrosing ILD on HRCT, 21 had a UIP pattern, 17 HAD a NSIP pattern, and two had NSIP associated with chronic obstructive pulmonary disease.
SP-D (21.91±2.17 versus 15.76±1.34 ng/mL; p=0.017), CCL-18 (102±13 versus 78±5 ng/mL; p=0.026), and KL-6 (961±128 versus 376±26 U/mL; p<0.001) concentrations (Figure 1A-C) were significantly higher in patients with RA-ILD versus unaffected patients with RA. KL-6 values were also higher in patients with UIP compared to the other HRCT patterns and in patients with lesion extensions >15% compared to patients with milder disease. Receiver operating characteristic curve analysis to assess the diagnostic abilities of the three markers for the diagnosis of RA-ILD showed a superiority of KL-6 (area under the curve [AUC]: 0.79; 95% confidence interval [CI]: 0.72–0.86), compared to SP-D (AUC: 0.66; 95% CI: 0.58–0.74), and CCL18 (AUC: 0.62; 95% CI: 0.53–0.70) (Figure 1D). The sensitivity of KL-6 for the diagnosis of RA-ILD was 68% with a specificity of 83%. In the French subset with longitudinal data (n=15), extension of ILD was detected in seven patients.
Baseline KL-6 serum levels were significantly increased in patients who experienced ILD progression (1,987±1,294 versus 799±375 U/mL; p=0.027) (Figure 1E). The degree of ILD progression on HRCT was also proportional to baseline KL-6 concentrations (Figure 1F).
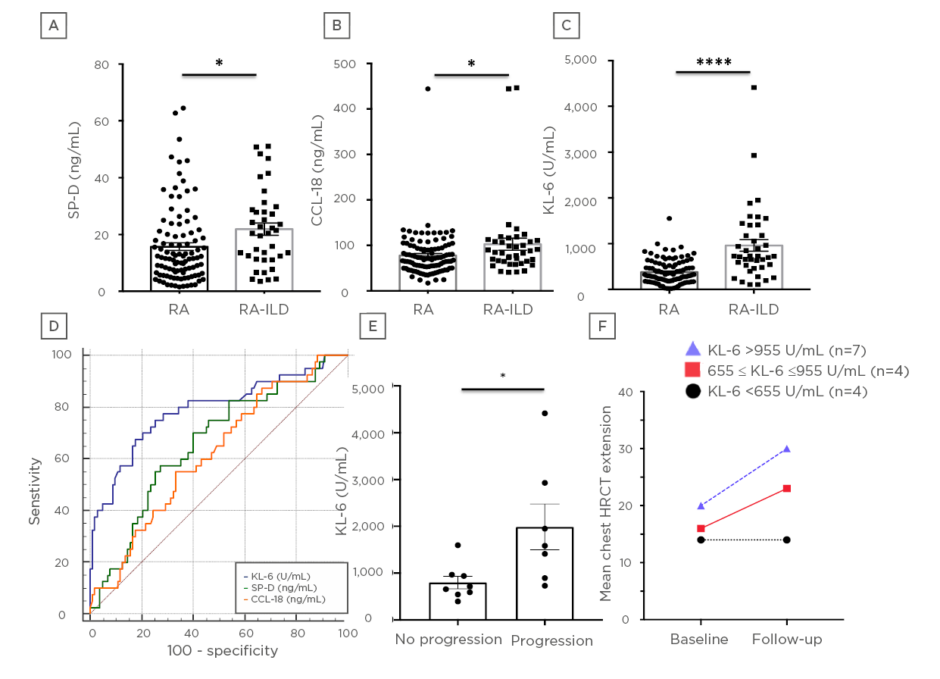
Figure 1: Concentrations of serum markers, diagnostic value, and performance of KL-6 for the progression of RA-associated ILD. A–C) Concentrations of SP-D (ng/mL) plus A) CCL-18 (ng/mL) and B) KL-6 (U/mL) and C) in patients with RA with or without associated ILD. D) Receiver operating characteristic curve illustrating the diagnostic value of SP-D, CCL-18, and KL-6 for diagnosis of ILD in patients with RA. E) Concentrations of KL-6 (U/mL) according to the progression on chest HRCT of RA-associated ILD. F) Degree of mean ILD progression on chest HRCT according to baseline KL-6 concentrations. The concentrations of 655 U/mL and 955 U/mL correspond to the first and second quartile of French patients with RA-ILD.
*p<0.05
**** p <0.0001 by Student’s t test.
CCL-18: C-C motif chemokine ligand-18; HRCT: high-resolution CT; ILD: interstitial lung disease; KL-6: Krebs von den Lungen-6 glycoprotein; RA: rheumatoid arthritis; SP-D: lung epithelial-derived surfactant protein-D.
CONCLUSION
KL-6 is relevant for the diagnosis and the prognosis of RA-ILD. It may be used as a circulating noninvasive first-line marker to stratify for indication of HRCT. Indeed, given the emerging lung issues in RA patients, this simple and highly reproducible marker, which is already available in routine care in some countries, could be a beneficial prerequisite to chest HRCT in rheumatology clinics.








