BACKGROUND AND AIMS
B-lines (BL) and pleural line alterations (PLA) are the typical lung ultrasound (LUS) findings for the detection and severity assessment of systemic sclerosis-associated interstitial lung disease (SSc-ILD).1-3 Recently, LUS scores have been shown to correlate with the extent of interstitial lung disease (ILD) and radiological abnormalities assessed by automated quantitative CT (qCT).⁴ Nevertheless, one of the limitations of LUS remains the ability to explore only the superficial areas of the lung parenchyma.
The aim of the study is to compare quantitative LUS scores with three-level qCT analysis (apices, midfields, and lung bases), and to evaluate their possible association with ILD extension of lung surface and core.
MATERIAL AND METHODS
During the period 2021–2023, patients with consecutive systemic sclerosis (SSc) underwent CT and LUS on the same day, performed by two blinded certified operators using the 14 intercostal space assessment technique.5 The total number of BLs was collected, and the quantitative PLA score proposed by the authors’ centre was applied, dividing each lung into three levels. CT images were assessed by two thoracic radiologists for ILD definition and then analysed via automated texture analysis software, quantifying the volumes of total ILD, ground-glass (GG), and reticulations (RET), also differentiating ILD volume of the lung surface and core.
RESULTS
Eighty-two patients were enrolled, with 59 (72%) presenting ILD on CT (Table 1A and 1B). The median number of BLs was one (0;4) for apices, 6.5 (1;16) for mid-fields, and 11 (3;26) for lung bases. Median PLA score of the apical, middle, and basal lung fields was one (0;2), five (2;8), and six (2;11), respectively. Detailed qCT analysis is reported in Table 1A.
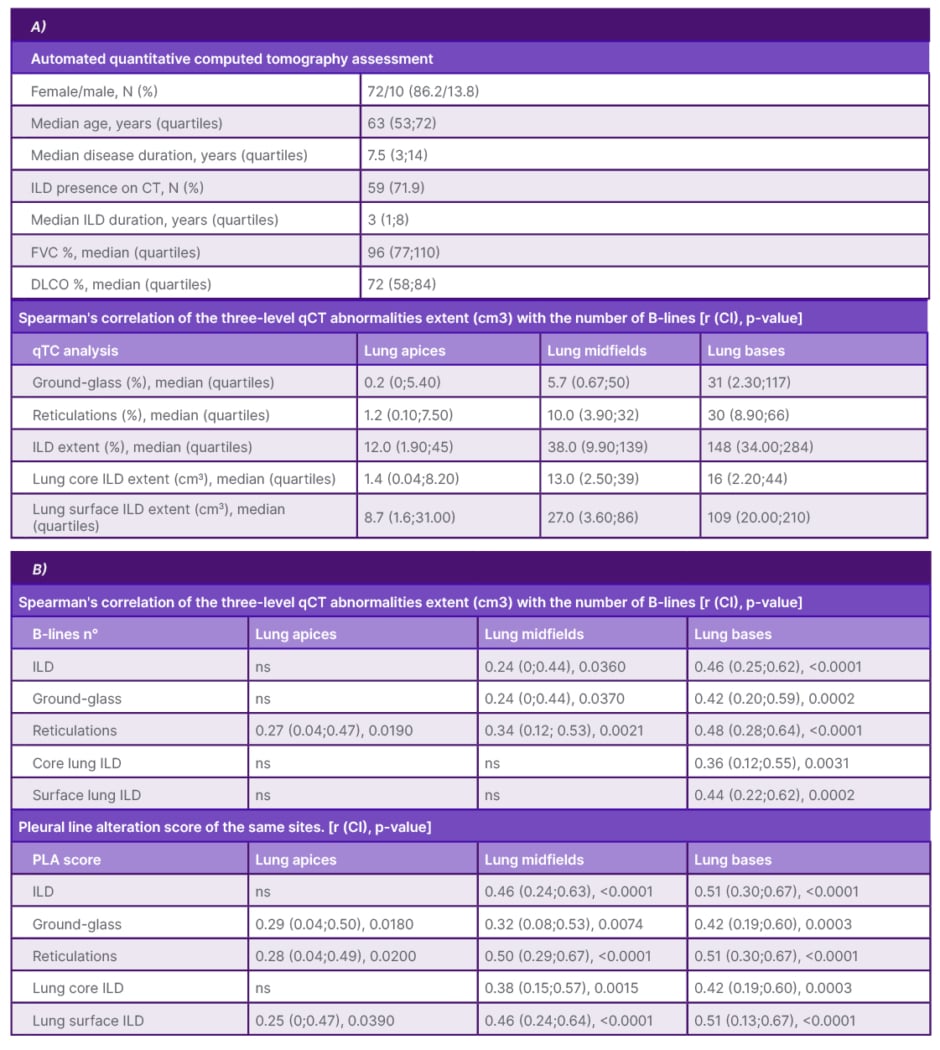
Table 1: A) Characteristics of study population and descriptive analysis of lung ultrasound and automated quantitative computed tomography assessment. B) Spearman’s correlation of the three-level qCT abnormalities extent (cm3) with the number of B-lines and with the pleural line alteration score of the same sites.
DLCO: diffusing capacity for carbon monoxide; FVC: forced vital capacity; ILD: interstial lung disease; N: number; PLA: pleural line alteration.
Both BL number and PLA score of mid-basal lung fields correlated with the extent of GG, RET, and ILD of the same level at qCT (p<0.005). The PLA score of lung apices correlated with the extent of GG and reticulations of the same site on qCT, whereas the number of BLs correlated only with RET (p<0.05). The extent of ILD, GG, and RET of the lung surface on qCT was significantly higher than the equivalent of the lung core (p<0.05). The basal lung BLs number was found to correlate with superficial and core ILD extent (p<0.005). The PLA score of the apices, mid-fields, and bases correlated with surface lung ILD, GG, and RET (p<0.05), and the mid-basal PLA score also correlated with deep lung alterations on qCT (p<0.02) (Table 1B).
CONCLUSION
The study confirms and expands on the recently emerged findings on the correlation of LUS with ILD extent at qCT, suggesting the ability of LUS to reflect lung morpho-structural changes, especially at basal lung, most affected by SSc-ILD. For the first time, LUS (particularly the PLA score proposed by the authors’ centre) was found to be associated with ILD volume of the lung core. This is probably because structural changes in the lung core would be reflected in the lung surface, where SSc-ILD is prevalent. These results may suggest the possibility of overcoming the traditional LUS limitation of investigating only the superficial lung parenchyma.







