Abstract
Papillary thyroid cancer (PTC) is an epithelial malignancy arising from the follicular cells within the thyroid, typically slow-growing with a benign course (5-year survival >99% in locally contained malignancies). However, in unusual cases, this condition can spread to the pleura, leading to a malignant pleural effusion. The authors present a case of an 80-year-old female presenting with dyspnoea following treatment for suspected bacterial pneumonia. Imaging revealed a substantial left-sided pleural effusion. Despite interventions such as thoracentesis and intravenous antibiotics, the pleural effusion persisted. Subsequent video-assisted thoracic surgery revealed pleural biopsies positive for PTC, a disease previously believed to have been cured almost 6 decades ago. Pleural involvement in patients with PTC is exceptionally rare. A literature review conducted between 1992–2023 revealed merely seven published reports documenting PTC metastasis to the pleura. The authors’ case emphasises the significance of exploring various potential causes of a patient showing signs of subacute dyspnoea, particularly in individuals previously diagnosed with PTC, as it emphasises the possibilities of unforeseen recurrence, featuring the uncertainties and complexities of managing PTC.
Key Points
1. Papillary thyroid cancer (PTC) is the most common thyroid malignancy, accounting for 80–85% of cases. It has a favourable prognosis with a 93% survival rate at 10 years, but recurrence and distant metastasis can still occur, impacting survival.2. Recurrence affects about 10% of PTC patients, influenced by factors like lymph node metastasis, tumour size, and patient age. While PTC commonly spreads to regional lymph nodes, distant metastases to bones or lungs occur in 1–4% of cases. Rarely, pleural metastasis with effusion can happen.
3. The manuscript presents a rare case of pleural metastasis in an 80-year-old patient, nearly 60 years after initial PTC treatment. This case emphasises the importance of thorough diagnostic evaluation in long-term PTC survivors presenting with dyspnoea and pleural effusion.
INTRODUCTION
Papillary thyroid cancer (PTC) is the most common form of thyroid cancer, accounting for 80–85% of thyroid cancer cases. Despite being the most frequent thyroid cancer, it has the best outcomes, and is rarely metastatic.1 PTC boasts a favourable survival rate; however, recurrence is a significant concern, affecting approximately up to 10% of patients at various stages of their lives.2 The average time to recurrence spans from 6 months to several decades later.3 Several factors have been identified as contributors to an elevated risk of recurrence, including, but not limited to, lymph node metastasis, histologic variant, tumour size, extrathyroidal extension, extra nodal extension, male gender, and an age >45 years at the time of initial diagnosis.3 PTC is one of the most treatable cancers relative to other differentiated and undifferentiated thyroid malignancies, boasting a survival rate of 93% at 10 years.4 Around 30–40% of PTC metastasises to regional lymph nodes. However, distant metastasis may occur and account for 1–4% of the patients, reducing the survival rates to 24–76%.5 In 5–10% of instances, distant metastasis may manifest in the bones or lungs, and in uncommon cases, it may occur in the pleura, accompanied by the accumulation of effusive fluid.5 While metastasis to the lungs is common, metastasis to the pleura with the collection of large amounts of fluid requiring thoracentesis is rare. In the last 5 years, fewer than five cases have been described. This case report describes a patient for whom a partial thyroidectomy was performed in 1965 for PTC, who presented to the hospital with progressively worsening subacute shortness of breath found to have a large pleural effusion due to unknown recurrent metastatic disease to the pleura.
CASE PRESENTATION
An 80-year-old female with a history of hypertension and papillary thyroid cancer, treated with subtotal thyroidectomy in 1965, presented to the emergency room with acutely worsening dyspnoea. Six weeks prior to presentation, she developed symptoms mimicking her husband’s respiratory syncytial virus infection, including a productive cough. She initially was seen at an urgent care centre 4 weeks prior to presentation, where an X-ray was performed and demonstrated a left lower lobe pneumonia. At that time, she was treated with oral amoxicillin/clavulanic acid, azithromycin, and prednisone. Despite initial improvement, her condition deteriorated, leading to severe breathlessness.
On presentation to the emergency department, vital signs included a blood pressure of 137/86 mmHg, heart rate of 62 beats per minute, temperature of 36.7 °C, respiratory rate of 19 breaths per minute, and oxygen saturation of 96% on 2 L via nasal cannula. Laboratory tests revealed an elevated D-dimer level, and normal troponin and procalcitonin levels. Computed tomography angiography was performed to exclude a pulmonary embolism, which was ruled out, but the imaging demonstrated a large left pleural effusion with compressive atelectasis (Figure 1A). The patient was admitted for respiratory failure secondary to a large left-sided parapneumonic effusion.
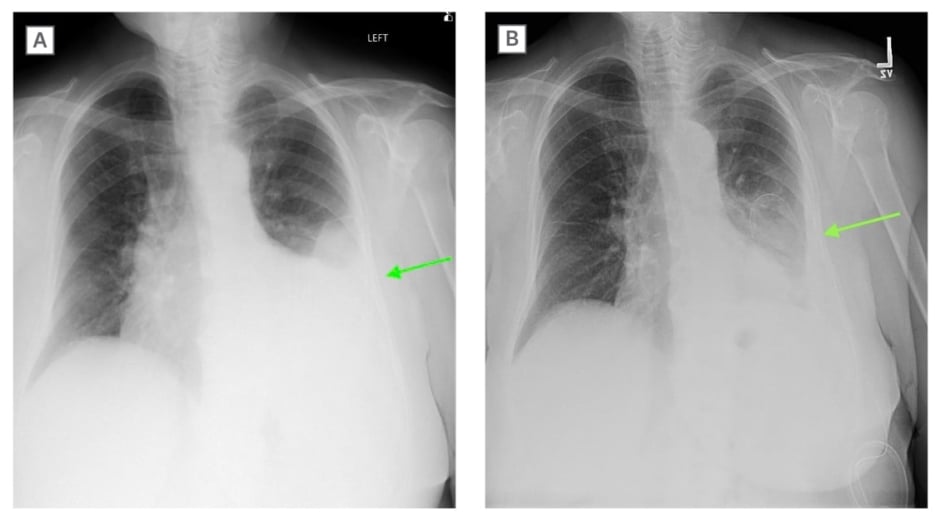
Figure 1A: Posteroanterior view of the chest on X-ray obtained on admission demonstrated a
moderate-large left pleural effusion (green arrow).
Figure 1B: Posteroanterior view of the chest on X-ray after video-assisted thoracoscopic surgery and pleural catheter insertion (green arrow).
While on the medical floor, the patient was evaluated by the in-house pulmonologist. Given the patient’s oxygen requirements and the large nature of the effusion, the decision was made to perform a thoracentesis. Pleural fluid studies established the effusion to be an exudative effusion (Table 1).
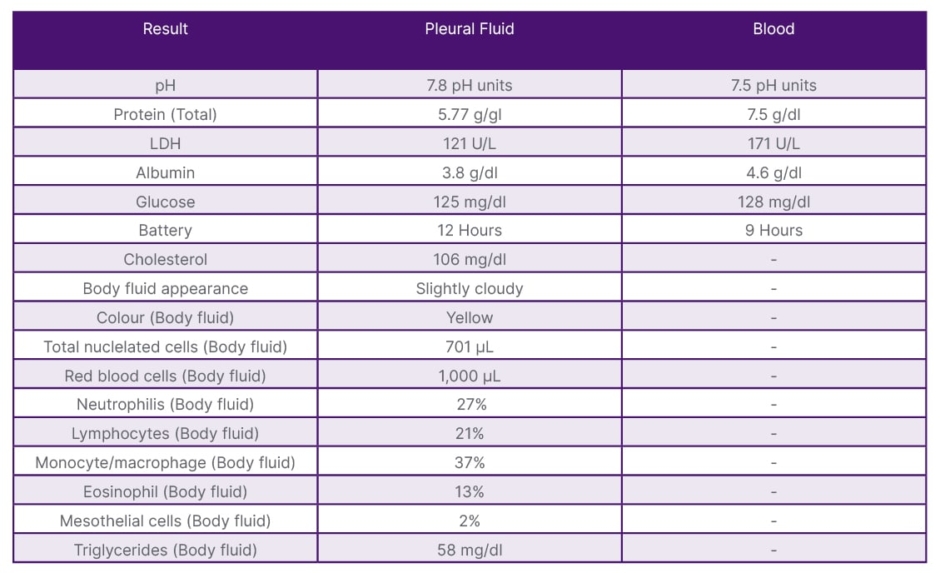
Table 1: Thoracentesis results.
However, prior to performing the thoracentesis, on point-of-care ultrasound, the effusion had characteristics consistent with a complicated effusion. After the procedure was performed, cardiothoracic surgery was consulted. They believed the effusion to still be parapneumonic, and recommended treatment with intravenous antibiotics and outpatient follow-up for resolution.
One month after discharge, the patient was noted to have a persistent pleural effusion. This led to the performance of video-assisted thoracic surgery (Figure 1B). Biopsies taken of the pleura during the procedure were positive for metastatic thyroid papillary cancer. This diagnosis comes nearly 60 years after the patient’s initial cancer treatment. After the procedure, a CT of the neck showed changes consistent with previous thyroid surgery and new nodules in the remaining thyroid lobe (Figure 2).
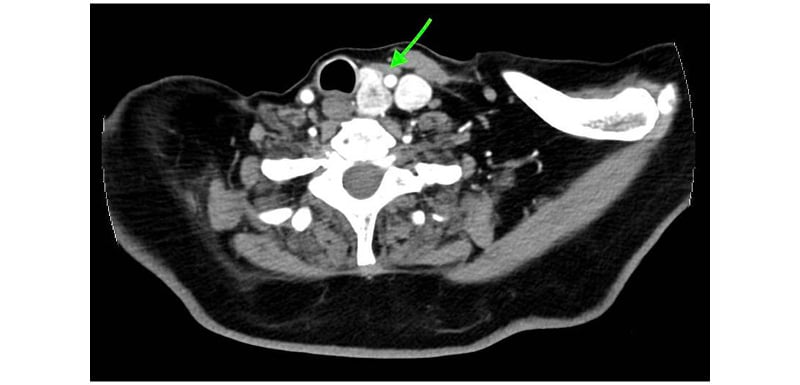
Figure 2: CT of the neck with intravenous contrast.
The CT of the neck with intravenous contrast demonstrated prior resection of the right thyroid lobe and isthmus, as well as right neck dissection. The left thyroid lobe was mildly enlarged and heterogeneous with several nodules measuring up to 1.5 cm (green arrow).
The patient subsequently underwent a PET/CT that showed focal fluorodeoxyglucose uptake within the medial aspect of a consolidated left lower lobe opacity, with a maximum standardised uptake value of 8.3, suspicious for biologic tumour activity. The patient was scheduled for total thyroidectomy with neck dissection, followed by radioactive iodine treatment with pleural catheter removal 4 weeks post-surgery.
DISCUSSION
PTC, an epithelial carcinoma, is the most common of thyroid malignancies, accounting for 80–85% of all cases.1 It is distinguished by follicular nuclear patterns and the ability to invade nearby lymphatic structures.6 Slow growing, PTC has the best outcomes of the thyroid cancer groups, with a 99.5% 5-year relative survival rate amongst all Surveillance, Epidemiology, and End Results (SEER) stages combined.7 The incidence is higher among women compared to men by a 3:1 ratio.8
Only 10% of cases of PTC present with metastatic disease.1 Per guidelines from the American Thyroid Association (ATA) and National Comprehensive Cancer Network (NCCN), a conservative approach in the form of a thyroid lobectomy is sufficient for low-risk disease. Low-risk disease is defined as having no prior history of radiation, no distant metastases, no cervical lymph node metastases, no extrathyroidal extension, and a tumour ≤4 cm in diameter.9 In the case of the authors’ patient, subtotal thyroidectomy was deemed appropriate in her case, as the tumour was 2 cm and had no extrathyroidal extension or lymph node involvement.
The rate of recurrence is difficult to ascertain as all re-operations on patients having already undergone subtotal thyroidectomy or thyroidectomy are labelled as recurrent disease without differentiation for persistent disease.3 Some indicators of persistent disease include re-operation within the first year of the initial surgery.3 One randomised retrospective study demonstrated only a 4.3% risk of recurrence, mostly in the neck lymph nodes, with a median time to recurrence of 56.8 months.10 This deviates from the authors’ patient as her reoccurrence occurred 720 months after her initial procedure. It is difficult to determine the exact time of recurrence as the patient stopped monitoring her thyroid function 10 years after she was disease-free.
The incidence of pleural metastasis originating from PTC stands at 0.6% of cases.11 It is often identified through pleural fluid analysis; however, the authors’ case veers from this as they had negative cytopathology results from thoracentesis. This initially negated the possibility of PTC recurrence. However, upon reviewing the pleural biopsy, the diagnosis of metastatic papillary thyroid cancer was conclusively established.
Metastasis of differentiated thyroid cancers, including papillary, is thought to be through lymphatic spread. Typically, metastatic spread starts in nearby lymph nodes before settling into faraway tissues. In papillary thyroid cancer the preferred metastatic sites (after the lymph nodes) include the lungs and the bones. This is due to the modification of the microenvironments of the target organ prior to the establishment of tumour cells. This alteration occurs due to cytokine-cell interactions, which are still poorly understood.4
CONCLUSION
This case emphasises the significance of exploring various potential causes of a patient showing signs of subacute dyspnoea. A thorough and accurate assessment of both medical and surgical history is vital in acquiring crucial details necessary for an exact diagnosis. For individuals previously diagnosed with PTC who encounter aggravated or new dyspnoea, or display a new pleural effusion, the potential of pleural metastasis should be considered. Furthermore, it emphasises the possibilities of unforeseen recurrence, featuring the uncertainties and complexities in managing PTC. Given that the patient was 60 years cancer-free, metastatic recurrence of her disease seemed unlikely. However, through thorough and invasive work-up, the correct diagnosis was found.
As the financial implications of medical practices become increasingly apparent, it is essential to acknowledge that initial investigations into pleural effusions should prioritise more prevalent and less complex aetiologies. Prematurely proceeding to invasive and costly interventions may adversely impact patient outcomes both personally and clinically. Clinicians must remain cognisant of the financial implications for patients, while emphasising the importance of thorough investigation to achieve an accurate diagnosis. Metastatic spread of papillary thyroid cancer is a negative prognostic factor, with multiple organ metastasis being associated with higher frequency of death (50.4%) versus single organ involvement (36.7%).4 The 5-year survival rate in patients with metastasis limited to one organ was 77.6%, while that in patients who develop second organ involvement was as low as 15.3%.12
New studies are aiming to use the presence of pleural effusion in metastatic disease as an independent prognostication factor outside the typical factors that are identified for a decrease in survival. This includes age >45 years, cancer with metastasis to bone, increased tumour size and tumour size >3 cm, and incomplete tumour resection.13 This case presentation aims to enrich the existing body of medical knowledge and contribute to the ongoing advancement of the field. By sharing a detailed clinical scenario, the authors hope to enhance understanding, foster informed decision-making, and encourage further research that may lead to improved patient care and treatment protocols.







